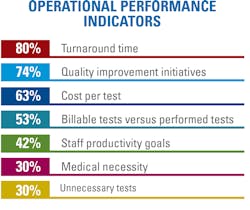
Lab administrators prioritize accurate and timely financial and operational performance
While clinical labs have long faced operational challenges and financial pressures, the magnitude of these issues during the COVID-19 pandemic has been unprecedented. Clinical lab administrators face shrinking reimbursements, staff shortages and supply chain disruptions at a time when test volumes are through the roof. The ability to perform accurate and timely analytics on operational and financial performance has never been more critical.
In our first of four “State of the Industry” survey topics for 2021, MLO explored clinical data analytics adoption among labs, including opportunities to leverage analytics to support lab operation and management, and factors holding them back from data-based performance improvement initiatives.
Among survey respondents, 62% are in leadership positions, such as lab managers, administrators, supervisors, lab directors and section/department managers, with most working in hospital labs. The remaining respondents represent a broad range of job functions across a variety of facilities and lab sizes.
The demand for advanced analytics
The role of clinical labs has evolved to meet the growing demands of healthcare. Their work goes far beyond the running of tests. Labs today must have the ability to support initiatives around value-based care and pay for performance. This means the capability to perform advanced analytics, says Tracy Roth, MBA, Senior Director, Product Management, Data and Analytics, Sunquest Information Systems:
“Long gone are the days of producing test results in the hospital basement. Today’s clinical laboratories are expected to lead evolving strategies in diagnostics, treatment and cost efficiency; these include optimizing operational effectiveness and test turnaround time, meeting value-based healthcare reimbursement targets, and exceeding consumer expectations. The practice of data analytics is at the core of these requirements and provides the roadmap for laboratory success.”
As healthcare in general has been forced to rethink its approach to patient care, labs too must transform their strategies to support new care delivery models, according to Kim Futrell, MT(ASCP), MSHI, Senior Strategic Marketing Manager, Orchard Software Corporation:
“Changes within the healthcare system are pressuring laboratory professionals to update their thinking and focus on a broader scope of laboratory stewardship. Laboratories are encouraged to find specific ways to contribute in a value-based, patient-centered healthcare system, which includes leveraging data analytics – supporting population health initiatives and determining downstream impact of laboratory contributions.”
With value-based care comes the demand for labs to generate information that can help healthcare organizations improve clinical effectives and care outcomes, explains Joseph Chiweshe, MD, MPH, Senior Manager at Beckman Coulter:
“We are in the midst of an expanding shift for our care models to improve the cost of healthcare and better align patient outcomes with impact for value. Organizations seek solutions that measure patient progress, provider performance and costs to advance health which are closely tied to lab operations, quality and management. Furthermore, COVID-19 has changed how labs must operate from having to implement contingency planning for at risk or infected staff in the face of existing labor shortages.”
The use of data analytics can help labs operate more effectively and efficiently at a time when their services are needed more than ever, says Jamie Gramz, Head of Digitalization from Siemens Healthineers:
“There are several factors that are driving the use of data analytics to assess and improve lab operations. These include the overall need to do more with less in order to address staffing challenges, reduce costs, improve turnaround times, satisfy compliance requirements and accommodate the increasing demand for laboratory testing.”
Moving beyond manual processes
In an effort to operate more efficiently and maximize existing staff resources, clinical labs have increasingly been transitioning from manual to electronic processes. As of January 1, 2021, Medicare is paying higher rates to labs that can turn around SARS-CoV-2 virus testing results within two calendar days of the specimen being collected;1 therefore, labs have a strong financial incentive to secure results faster.
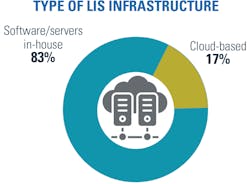
With regards to their LIS platforms, 61% of respondents say their labs use a module within an enterprise-wide electronic health record system, while 39% use stand-alone systems. A growing number of labs are adopting cloud-based LIS systems (17%), with 83% still using in-house software/servers.
“Open connectivity and the use of middleware play a key role in empowering labs to interface analyzers from the manufacturer of their choice for multidisciplinary testing,” said Gramz. “By leveraging integrated data management, labs can also visualize testing status with alerting capabilities to help to create awareness and drive action.”
Although labs are increasingly integrating internal systems and adopting cloud-based technologies, more than half (53%) say interoperability and data integration issues with LIS or electronic health records are still “stumbling blocks” to implementing electronic processes.
“To overcome these challenges, the important first step is to clearly define the data and analytic needs of the laboratory, as well as those of stakeholders and how they align with the health systems goals and needs” said Roth. “Then, collaborate with trusted technology partners to bridge this gap. This partner must be well-versed in the complexities of laboratory workflow and data output.”
Clinical lab leaders recognize the critical role of technology in supporting operations, and the need for improvements in this area. When asked to name their strategic priorities for their organizations in the next three years, the two top ranking responses were infrastructure and platform development (31%) and data analytics optimization to support lab management (25%).
Rick Callahan, VP Sales and Marketing, NovoPath, recommends purchasing laboratory equipment and software that conforms to HL7 (Health Level-7) standards to support standardization of data sharing between systems. He also recommends selecting hardware and software vendors that have previously worked together on interfacing their solutions in order to pave the way for system integration.
- Help clinicians identify abnormal and clinically actionable results
- Reduce waste and operational redundancies
- Cater to quality metrics that reward performance
- Assist with change in volume demand
- Improve speed and accuracy of patient test results
- Maintain standardization across the system
“Lastly, if you should employ a third party to develop interfaces with your software/hardware, hire an organization that is well established and experienced,” said Callahan. “They are more likely to have interfaced to the same hardware/software that you are trying to interface with. ”
Data-driven decisions
Those labs with access to accurate, timely and comprehensive data have the ability to perform advanced analytics for continuous improvement. According to Chiweshe, some of the benefits that clinical labs can gain from advanced analytics include:
- Increased efficiency and effectiveness of lab operations and patient care2
- Optimized costs
- Improved turnaround times
- Increased workflow efficiency
- More efficient use of staff time
- Better collaboration with healthcare partners outside the laboratory
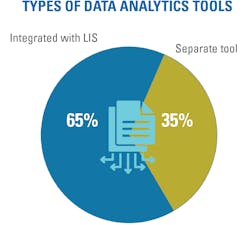
The survey revealed that most clinical labs use analytics to support lab operations. More than half (66%) of those surveyed said they use data analytics for at least some aspects of lab management, with 11% using analytics for all aspects, and 53% using it for some and planning more. The majority of labs use data analytics tools that are integrated with their LIS (65%), while 35% use a separate tool.
The reliability and usefulness of analytics are only as good as the data backing them. The fresher the data, the more relevant the results. Among those using data analytics in their operations, nearly one-third (29%) say they use real-time data, 10% say their data is refreshed by hours/minutes, 28% daily and 33% weekly.
“We are looking at a future where IT systems can analyze databases with genome analyses from hundreds of patients for trends that aid in determining the best treatment plans,” said Futrell. “This future role of the laboratorian is expected to shift away from specimen handling toward data processing and interpretive guidance.”
COVID-19
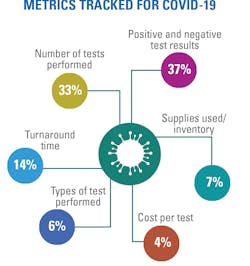
When asked what metrics their labs are tracking specific to COVID-19, the top areas were positive and negative test results (37%) and number of tests performed (33%), followed by turnaround time (14%), suppliers used/inventory management (7%), type of test performed (6%) and cost per test (4%).
The COVID-19 pandemic has elevated the importance of analytics, according to Carl Smith, General Manager, Lab Division, CompuGroup Medical U.S.
“Due to the COVID-19 pandemic, analytics have become more important than ever,” said Smith. “Labs are the healthcare industry’s key resource for proper diagnosis and treatment. As vendors, we need to ensure that all data is accessible. We must provide the data analytics needed to assist with the current situation and establish the systems that will empower laboratories to manage all future pandemics.”
One area that has been hit hard by the pandemic is staffing, explains Callahan, prompting many labs to “rethink” how they operate. He states:
“Some facilities are working with reduced staff due to hiring freezes imposed by management, employees working from home, attrition and quarantined personnel. These labs need to analyze the way they do business, and with the results of the analysis, ‘rethink’ the way they have done business in the past, so that they can ensure patient safety, accurate results, timely turnaround time, as well as their external client’s satisfaction.”
Planning and forecasting
Visibility into existing processes, supplies and staffing are necessary for labs to identify shortcomings, gaps and waste, and plan accordingly for the future to boost operational and financial performance. When it comes to management forecasting, test utilization was highest on the list (67%) of tests that labs perform, followed by workloads (60%), staffing levels (54%) and supply utilization (43%).
The majority (68%) of labs use an electronic tool for management forecasting. About half (54%) incorporate data from other departments (e.g., finance, ED, inpatient units) into measurement for performance improvement initiatives or planning for capital expenditures.
As Roth points out, advancements in analytics and the ability to better plan and forecast offers ways for a clinical lab to differentiate itself from the competition.
“Laboratory results are a critical component of patient diagnostics, treatment decisions and disease surveillance,” said Roth. “Accessible data and timely metrics offer laboratories a differentiator – the opportunity to identify drivers of efficiency, optimize their revenue models, plan for future changes in volume, and create their value story within the healthcare ecosystem. Additionally, transformative laboratory analytics can anticipate changes in patient acuity and population health risk, which ultimately leads to improved physician decision-making, patient health outcomes and cost efficiency.”
The road ahead
The healthcare industry has long struggled to adapt to value-based care and payment models, with a growing reliance on clinical labs to provide analytics to support data-driven decisions. The emergence of COVID-19 has only added fuel to the fire as labs, already facing staffing shortages and pressures to operate more efficiently, have been pushed to their limits.
In order for clinical labs to meet current and future demands in patient care, Futrell says they must break down existing barriers and proceed with a more holistic approach, stating:
“Laboratory professionals and healthcare workers in general must stop thinking and functioning in silos and think in terms of patient-centered care. Secondly, laboratories need an informatics partner that can integrate everything lab-related across their organization. Partner with your IT staff to gain an understanding of how the lab system fits within the overall organizational architecture.”
Futrell also believes that optimal use of laboratory data can help laboratory professionals gain greater visibility, recognition and respect that has long been denied.
In looking towards the future, Smith references how clinical labs are embracing the Clinical Lab 2.0 movement, with its focus on data analytics as a way to support value-based care. In describing this movement, the Clinical Lab Management Association (CLMA) explains how leading health systems are leveraging “the massive real-time data emanating from their in-system laboratory services to drive better patient outcomes on a more cost-effective basis, close gaps-in-care, and improve revenue cycle and value-based payments at the system level.”3
“We work with industry experts and clients to build a platform for the Lab 2.0 concept, which emphasizes using laboratory data to produce actionable insight that can lead to better patient outcomes,” says Smith. “For example, CGM develops customized reporting for its lab clients. Armed with these reports, labs can provide physicians with the analytics to assist with predictive modeling, improving the long-term care that patients receive.”
For clinical laboratories wanting to improve their operational workflow and achieve optimal lab administration, Callahan recommends taking a Lean Six Sigma approach.
“While I would recommend that you conduct a thorough Six Sigma Analysis for the entire laboratory operation, this process is very time consuming,” said Callahan. “You can instead break down the lab into functional ‘areas’ and select areas one at a time to focus in on and work the Six Sigma process.”
REFERENCES
- CMS Changes Medicare Payment to Support Faster COVID-19 Diagnostic Testing CMS, October 15, 2020, https://www.cms.gov/newsroom/press-releases/cms-changes-medicare-payment-support-faster-covid-19-diagnostic-testing. Accessed January 11, 2021.
- Moore E. A systematic review of the imapact of health information technology on nurses’ time. JAMIA.1;27(5): 798- 807. doi: 10.1093/jamia/ocz231.
- Clinical Lab 2.0: What is it? How Does This Translate into Laboratory Management and Leadership? CLMA. https://www.clma.org/p/bl/et/blogaid=557. Accessed January 11, 2021.