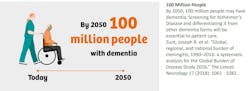
The neurodegenerative processes that precede dementia begin to chip away at a person’s cognitive reserve many years before mental capacity is determined to be outside the normal population range.1 Mild cognitive impairment (MCI) represents a state of partial decline that may be evaluated by neuropsychological testing but falls short of the criteria for dementia. Alzheimer’s disease (AD) is the most common form of dementia and affects an estimated 6.9 million Americans above the age of 64.2 In Europe, more than 10 million people are affected by MCI and roughly half are expected to progress to dementia within 5 years.3 Due to the lack of routine cognitive screening, 50% to 70% of patients with symptoms of AD are not recognized or diagnosed in primary care.4 For early onset AD, in which patients and those around them are less likely to consider medical help, diagnosis may be delayed 2-3 years.5 The diagnostic process is even less effective for those with subjective or mild cognitive impairment (See Figures 1, 2, 3). Therefore, more effective diagnostic solutions are needed. To facilitate the advancement of new solutions, numerous research projects are currently underway. This article provides a brief introduction to some recent initiatives.
The AI-Mid Connector project has enrolled more than half of its planned 1,000 patients in a study of AI tools for prediction of their risk to develop dementia based on high-density magneto- and electroencephalography combined with cognitive tests and genetic biomarkers.6 Wider use of wearable technologies for tracking physical activities, speech, and other biomarkers provides additional possibilities for detecting patterns that may relate to onset of dementia.
The CUBOId study was designed to acquire data from wearables and other fixed sensors from participants diagnosed with MCI or AD and their live-in partners in the United Kingdom. Deep learning methods will be utilized to analyze activity and speech patterns.7 Observed behaviors that may be relevant to cognitive decline include patterns of room occupancy, wandering and partner shadowing, and sleep disturbances.
RADAR-AD is a European project funded by the Innovative Medicines Initiative8 focusing on use of technology to monitor the impact of AD on daily functioning. Its goal is to understand how AD affects daily activities and to explore how technologies like smartphones and sensors can track these changes. This project will involve research with 220 AD patients across Europe. It builds on previous work by the RADAR-AD consortium, which focused on developing a biomarker screening platform and identifying biosignatures for early AD diagnosis and interventions.11
A project incorporating a wholistic approach to determining an individual’s risk of dementia, entitled PREDICTOM (Prediction of Neurodegenerative Disease using a Biomarker Screening Platform), recently secured funding for a consortium of 30 partner organizations to develop an AI-based screening platform to identify individuals at risk of developing dementia, even before symptoms manifest. Identifying risks associated with AD is crucial for early diagnosis, as it enables timely interventions for early detection. Moreover, early identification of risk factors not only aids in prompt initiation of treatments but also maximizes the effectiveness of new disease-modifying therapies (DMTs) designed to target the early stages of the disease. A major goal of their approach is to enable individuals to perform screening themselves in the comfort of their homes. More than 4,000 participants will be enrolled in the initial trial. This will include individuals from previous projects including PROTECT UK, PROTECT Norway, and Radar-AD, as well as others. In addition to home collection of blood samples and use of digital biomarkers, additional laboratory tests, magnetic resonance imaging, and electrophysiological testing will be utilized to develop a generalized risk assessment method to prioritize access to preventative measures and to aid in earlier diagnosis and prognosis.9
One overall aim for such projects is to provide primary care physicians with the tools they need to assess disease risk for those in their care, and to also provide easily interpreted evidence for decisions leading to more efficient and effective follow up through specialists. Because there is no cure for AD today, care must be taken to understand how a diagnosis of dementia may affect various aspects of a person’s life. Strained relationships, continuing employment, access to healthcare, and psychological outcomes must all be considered. Such an undertaking requires a wide range of capabilities. As part of the Innovative Health Initiative, which is a European public-private partnership, a group of 30 academic, governmental, and industry partners are working in a consortium spanning Europe, Asia, and the Americas. Advances at this scale of effort do not come cheaply and a total of €21M will be provided from November 2023 through to October 2027 to complete this work.
Several reasons for being optimistic that such groundbreaking work may lead to positive results exist:
- Advances in diagnostics methods: The ability to use self-collected capillary blood or interstitial fluid samples for health tracking increases the accessibility of fluid biomarkers for applications like screening for AD. Data on the collection of finger prick blood for biomarkers of neurodegeneration, in a manner similar to what is done for self-testing of glucose levels by diabetics, was presented recently.10
- Advancements in AI and machine learning: These technologies have matured significantly, enabling more accurate and nuanced analysis of complex multi-modal data.
- Widespread wearable device usage: With the ubiquity of fitness trackers, smartphones, and other technologies allowing personal monitoring, they are more easily adopted for clinical applications.
- Greater health and wellness awareness: Society is more aware of and proactive about cognitive health, increasing the demand for accessible monitoring tools.
- Clinical validity of new testing methods: Blood-based biomarkers have shown tremendous potential in early identification of neurodegenerative diseases. This combined with recent developments in digital biomarkers provides a strong foundation for success.
Transitioning from CSF (cerebral spinal fluid) to blood-based biomarker tests is game changing because they are less invasive, more accessible, cost-effective, and highly scalable. This transition is already underway and well documented in the context of specialized research institutions offering such testing today. Wider availability is expected to enable a precision diagnostic approach in neurology akin to what was established in the fields of molecular virology and oncology in past decades. With clinical validation of scalable solutions, it is expected that use in memory clinics and primary care will be possible soon. While challenges exist, most notably in standardization of testing methods and development of kits for the highly automated, random-access instruments that are utilized in centralized laboratories, it is reasonable to assume that such tests will be used routinely in the near future.11
An interesting aspect of the PREDICTOM project is that, while it takes a practical and cost-effective approach to bringing diagnostics closer to the patient, it will also evaluate the most innovative technologies for risk identification — including advanced MRI methods, supplementary tools such as EEG and eye-tracking, and the utilization of blood-based biomarkers for comprehensive assessments. AI models will not only be used for data analysis, but also to direct those at high risk for dementia to personalized interventions that may slow or prevent further cognitive decline, and hopefully to prevent development of dementia.
Such a solution could enable those at risk for dementia to better plan in partnership with caregivers before a decline in mental capacity restricts their ability to make decisions. Furthermore, it could support preventative screening or more frequent disease monitoring, allowing for early interventions when DMTs are most potent. Pharmaceutical developers are investigating the utilization of DMTs in the pre-clinical or prodromal stage of disease, signaling a potential shift to a more proactive approach.
Beyond the direct personal impacts, the societal burden of dementia is significant. The care provided by family and other unpaid caregivers to dementia patients in the United States was recently estimated to be $339.5 billion. These costs combined with payments for professional services related to elders with dementia, raises the total to more than half a trillion dollars. Therefore, the returns in societal savings from earlier and more effective interventions could be significant.
Author Disclosures: Arejas J. Uzgiris is an employee of Siemens Healthcare Diagnostics Inc. and Gaby Marquardt is an employee of Siemens Healthineers AG. Both legal entities, Siemens Healthcare Diagnostic Inc and Siemens Healthineers AG are part of Siemens Healthineers, which is a partner in the PREDICTOM consortium. Arejas J. Uzgiris also owns stock in Siemens Healthineers, Siemens AG, and Bayer. Gaby Marquardt owns stocks in Siemens Healthineers and Siemens AG.
Acknowledgements: The authors would like to acknowledge several individuals for their review of the content for this article, including Lance Ladic and Thomas Benkert at Siemens Healthineers; Dag Aarsland at King’s College, London; and Nicholas Ashton at Banner Healthcare, Arizona.
References
1. Rossini PM, Miraglia F, Alù F, et al. Neurophysiological Hallmarks of Neurodegenerative Cognitive Decline: The Study of Brain Connectivity as A Biomarker of Early Dementia. J Pers Med. 2020;30;10(2):34. doi:10.3390/jpm10020034.
2. 2024 Alzheimer's disease facts and figures. Alzheimers Dement. 2024;20(5):3708-3821. doi:10.1002/alz.13809.
3. Haraldsen IH, Hatlestad-Hall C, Marra C, et al. Intelligent digital tools for screening of brain connectivity and dementia risk estimation in people affected by mild cognitive impairment: the AI-Mind clinical study protocol. Front Neurorobot. 2024;5;17:1289406. doi:10.3389/fnbot.2023.1289406.
4. Hansson O, Edelmayer RM, Boxer AL, et al. The Alzheimer's Association appropriate use recommendations for blood biomarkers in Alzheimer's disease. Alzheimers Dement. 2022;18(12):2669-2686. doi:10.1002/alz.12756.
5. Stojković T. Survival and pharmacotherapy delay in young onset Alzheimer’s disease. Alzheimer’s & Dementia. 2023;19.
6. Ai-mind.eu. Accessed May 28, 2024. https://www.ai-mind.eu/blog/ai-mind-passes-the-mark-of-500-research-participants-for-its-clinical-study/.
7. Kumpik DP, Santos-Rodriguez R, Selwood J, et al. A longitudinal observational study of home-based conversations for detecting early dementia: protocol for the CUBOId TV task. BMJ Open. 2022;23;12(11):e065033. doi:10.1136/bmjopen-2022-065033.
8. Homepage. IMI Innovative Medicines Initiative. Accessed May 28, 2024. https://www.imi.europa.eu/.
9. Gonzalez-Ortiz F, Kac PR, Brum WS, et al. Plasma phospho-tau in Alzheimer's disease: towards diagnostic and therapeutic trial applications. Mol Neurodegener. 2023;16;18(1):18. doi:10.1186/s13024-023-00605-8.
10. Huber, H. et al. A finger prick collection method for detecting blood biomarkers of neurodegeneration — a pilot study (DROP-AD). AAIC Abstr. 80275 (2023).
11. Lista S, Mapstone M, Caraci F, et al. A critical appraisal of blood-based biomarkers for Alzheimer's disease. Ageing Res Rev. 2024;96:102290. doi:10.1016/j.arr.2024.102290.
12. https://www.radar-ad.org/patient-engagement/radar-ad-nutshell
Figures 1, 2, 3 Empowering clinicians to transform Alzheimer's Disease management - Siemens Healthineers USA (siemens-healthineers.com) The page is copyrighted as follows: Siemens Medical Solutions USA, Inc. ©2024.