Gene-based therapy restores cellular development and function in brain cells from people with Timothy syndrome
In a proof-of-concept study, researchers demonstrated the effectiveness of a potential new therapy for Timothy syndrome.
The treatment restored typical cellular function in 3D structures created from cells of people with Timothy syndrome, known as organoids, which can mimic the function of cells in the body. These results could serve as the foundation for new treatment approaches for the disorder. The study, supported by the National Institutes of Health (NIH), appears in the journal Nature.
Sergiu Pasca, M.D., and colleagues at Stanford University, Stanford, California, collected cells from three people with Timothy syndrome and three people without Timothy syndrome and examined a specific region of a gene known as CACNA1C that harbors a mutation that causes Timothy syndrome. They tested whether they could use small pieces of genetic material that bind to gene products and promote the production of a protein not carrying the mutation, known as antisense oligonucleotides (ASOs), to restore cellular deficits underlying the syndrome.
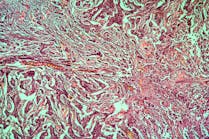
In the lab, researchers applied the ASOs to human brain tissue structures grown from human cells, known as organoids, and tissue structures formed through the integration of multiple cell types, known as assembloids. All of the methods were created using cells from people with Timothy syndrome. Applying the ASOs restored normal functioning in the cells, and the therapy's effects were dose-dependent and lasted at least 90 days.
The genetic mutation that causes Timothy syndrome affects the exon 8A region of the CACNA1C gene. The gene contains instructions for controlling calcium channels—pores in the cell critical for cellular communication. The CACNA1C gene in humans also contains another region (exon 8) that controls calcium channels but is not impacted in Timothy syndrome type 1. The ASOs tested in this study decreased the use of the mutated exon 8A and increased reliance on the nonaffected exon 8, restoring normal calcium channel functioning.