Patients with pancreatic cancer who received chemotherapy both before and after surgery experienced longer survival rates than would be expected from surgery followed by chemotherapy, according to a new study from researchers at Yale Cancer Center (YCC) and Yale School of Medicine.
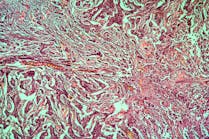
The study, published June 20 in JAMA Oncology, included patients with pancreatic ductal adenocarcinoma (PDAC), which accounts for 90% of pancreatic cancers.
The findings, say the researchers, are encouraging for the 15 to 20% of patients with pancreatic cancer whose tumors are operable.
The single-arm (only one treatment type or regimen) Phase II trial evaluated a modified form of the chemotherapy treatment FOLFIRINOX (a combination treatment consisting of leucovorin calcium, fluorouracil, irinotecan hydrochloride, and oxaliplatin approved in 2011 as a first-line treatment for patients with metastatic pancreatic cancer). Patients in the trial received six cycles of the modified FOLFIRINOX before surgery, followed by an additional six cycles of the chemotherapy treatment after surgery. The modified regimen consisted of slightly lower doses of FOLFIRINOX to improve tolerability, which was previously shown in a 2016 publication not to impact outcomes negatively.
Of the 46 patients who started the modified treatment, 37 completed all six cycles of chemotherapy before surgery and 27 had successful tumor removal operations. For all enrolled patients, the 12-month progression-free survival rate — meaning the disease did not worsen — was 67%, indicating significant progress in controlling the disease. Furthermore, 59% of all patients lived at least two years after completing the full chemotherapy treatment plan and surgery.
The study goal had been a 12-month progression-free survival rate of at least 50% of patients.
The study used advanced techniques to monitor the progress of treatment, including analyzing circulating tumor DNA (ctDNA) and using the cancer biomarker keratin 17 to help predict outcomes. For example, patients with detectable ctDNA four weeks post-surgery had significantly worse progression-free survival than those who had no detectable ctDNA.