A new treatment approach using an older drug may enable more patients with high-risk blood cancers to receive transplanted stem cells from unrelated, partially matched donors, according to a study conducted by researchers at Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine and colleagues.
Results to be presented at the annual meetings of the American Society of Clinical Oncology (ASCO) and the European Hematology Association suggest the new approach may expand the donor pool, with patients from underrepresented racial and ethnic groups standing to benefit the most.
Finding a matched donor has long been a major hurdle for patients with blood cancers who need bone marrow or blood stem cell transplants.
Patients without an eligible family member often turn to the National Marrow Donor Program. The registry contains more than 40 million potential donors, but not everyone finds a match, particularly people from underrepresented racial and ethnic groups. Only about half of Hispanic and a quarter of Black patients can find a fully matched donor, compared with more than 70% of white patients.
But the search for a donor has become a lot easier with the repurposing of cyclophosphamide, an older drug. The new approach – administering cyclophosphamide several days after transplantation – is leading to successful outcomes. New data will be presented May 31 at the ASCO meeting, with findings showing high rates of success in patients receiving blood stem cells from unrelated, partially matched donors.
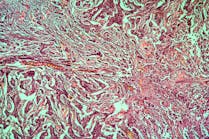
The new study assesses cyclophosphamide treatment in patients receiving peripheral blood stem cell (PBSC) transplantation. This stem cell source has largely supplanted bone marrow transplantation, partly because of the ease of donation via a procedure that collects the cells from the blood.
In this initial phase of the study, the researchers examined data from 70 adult patients with advanced blood cancers. Patients received a “reduced-intensity” conditioning regimen to prepare them for transplantation, followed by stem cells from unrelated, partially matched donors.
At ASCO, the researchers will report an overall high survival rate of 79% at one year, comparable to survival rates seen with fully matched donors. Other metrics were also promising, Jimenez Jimenez said. After one year, 51% of patients were free of GVHD and had not relapsed.
Donors had match levels from 4/8 to 7/8 on a one-to-eight scale, in which eight corresponds to a perfect match across eight key HLA markers. At match levels of 5/8 and above, more than 99% of people from a wide range of racial/ethnic groups are expected to find a donor.
The new findings are part of an ongoing phase 2 study enrolling about 300 patients at more than 30 medical sites, including Sylvester. Patients in a second arm of the study are receiving a more intense regimen prior to transplant, designed to ablate the bone marrow. A third arm investigates pediatric patients.