Cervical cancer kills more than 300,000 women annually. Global data from 2018 indicated that cervical cancer is the fourth most common female cancer, claiming an estimated 270,000 lives annually.1 It is well established that high-risk human papillomavirus (HPV) is the cause of almost all (99%) cervical pre-cancers worldwide.2
HPV is the most prevalent sexually transmitted infection in the United States. The virus currently affects 79 million Americans and is most commonly spread through vaginal or anal sex.3
Effective strategies for cervical cancer screening are available. A cytology-based test, the Pap smear, detects abnormal cells in the cervix, while HPV tests detect the presence of high-risk HPV genotypes in cervical cells. The American College of Obstetricians and Gynecologists (ACOG) endorses the U.S. Preventive Services Task Force (USPSTF) recommendations for cervical cancer screening. In women 30-65 years old, the USPSTF recommends the use of cytology-based testing every three years, primary high-risk HPV testing every five years with an assay approved by the U.S. Food and Drug Administration (FDA), or co-testing (high-risk HPV testing and cytology) every five years.4
There are more than 100 different genotypes of HPV. The low-risk types can cause genital warts, but the high-risk types can progress to cervical pre-cancer and cancer, with some of the high-risk types more likely to progress to cervical cancer than others.5 As the population vaccinated against HPV increases, decreases in HPV 16 and 18 can be seen,6,7 making it crucial to identify the other high-risk HPV types.
There are 14 genotypes that are considered high-risk and can lead to the development of cervical cancer and its precursor lesions: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68.8 The prevalence of high-risk HPV genotypes varies in cervical cancer cases. Of the 14 high-risk HPV genotypes, 16,18, and 45 cause 77% of cervical cancers worldwide. HPV types 16, 18, 45, 33, 58, 52 and 31 contribute to 90% of all cervical cancer. HPV types 51, 35, 39, 68, 56, 59, and 66, contribute to less than 9% of all cervical cancer.9
In a large clinical trial of a currently FDA-approved HPV assay with extended genotyping, the occurrence of cervical disease in 33,858 women 21 years and older was tracked during routine cervical cancer screening. High-risk HPV was detected in 15% of the cases.10
Researchers compared prevalence of HPV genotypes in samples with a negative histology result with those with severe disease, which is defined as cervical intraepithelial neoplasia disease of 3 or worse (CIN3+). Based on those parameters, 16, 18, and 31 were the most prevalent genotypes in cases of CIN3+.10
HPV assays
Because not all high-risk HPV types pose the same risk for cervical pre-cancer and cancer, HPV assays often report out information regarding individual HPV genotypes. Some HPV assays offer partial genotyping, reporting HPV 16 and 18 or 18/45 separately, and the remaining high-risk HPV genotypes in a pooled report. HPV assays with extended genotyping detect at least five individual high-risk HPV genotypes, such as HPV 16, 18, 31, 51 and 52.11
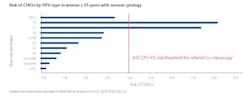
Reporting some high-risk HPV genotypes in a pooled report may mask the true risk of (CIN3+), particularly for HPV 31, which poses a similar risk for cervical pre-cancer and cancer, as compared to HPV 18. That is why pooled reporting of high-risk genotypes, such as 31, can lead to a one-year follow-up recommendation instead of an immediate colposcopy referral.12,13,14
Knowing the HPV genotype of an infection is critical in assessing patient risk. As seen in Figure 1, the risk of CIN3+ in HPV positive women over 25 years old with normal cytology varies, depending on which genotypes are detected in a patient’s specimen.14
The goal of cervical cancer screening is to detect pre-cancer, before it develops into cancer. HPV tests that offer extended genotyping provide a more personalized assessment of an individual’s risk for developing cervical pre-cancer and cancer.
References:
- World Health Organization. Cervical Cancer. https://www.who.int/health-topics/cervical-cancer#tab=tab_1. Accessed 7/21/2021.
- Meites E, Gee J, Unger E, Markowitz L. Human Papillomavirus. Centers for Disease Control and Prevention. https://www.cdc.gov/vaccines/pubs/pinkbook/downloads/hpv.pdf. Accessed Juy 21, 2021.
- Centers for Disease Control and Prevention. Genital HPV Infection – CDC Fact Sheet. https://www.cdc.gov/std/hpv/hpv-Fs-July-2017.pdf. Accessed July 21, 2021.
- American College of Obstetricians and Gynecologists. Updated cervical cancer screening guidelines. Practice Advisory. Washington, DC: American College of Obstetricians and Gynecologists; 2021. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2021/04/updated-cervical-cancer-screening-guidelines. Accessed August 10, 2021.
- HPV and HPV Testing. American Cancer Society. https://www.cancer.org/cancer/cancer-causes/infectious-agents/hpv/hpv-and-hpv-testing.html. Accessed July 20, 2021.
- Wright T, et al. HPV infections and cytologic abnormalities in vaccinated women 21-34 years of age: Results from the baseline phase of the Onclarity trial. Gynecol Oncol. 2019 May;153(2):259-265. doi: 10.1016/j.ygyno.2019.02.016.
- Drolet M, et al. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: updated systematic review and meta-analysis. Lancet. 2019 Aug 10;394(10197):497-509. doi: 10.1016/S0140-6736(19)30298-3.
- Human papillomavirus (HPV) and cervical cancer. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer. Accessed August 10, 2021.
- Sanjose S, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010 Nov;11(11):1048-56. doi: 10.1016/S1470-2045(10)70230-8.
- Stoler M, Wright T, Parvu V, et al. The Onclarity human papillomavirus trial: design, methods and baseline results. Gynecol Oncol.2018; 149(3):498-505. doi: 10.1016/j.ygyno.2018.04.007.
- Bonde, J, Ejegod, D, Cuschieri, K, et. al. The Valgent 4 protocol: robust analytical and clinical validation of 11 HPV assays with genotyping on cervical samples collected in SurePath medium. J Clin Virol. 2018 Nov;108:64-71. doi: 10.1016/j.jcv.2018.09.012.
- Perkins R, et al. 2019 ASCCP risk-based management consensus guidelines for abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis. 2020;24:102-131. doi: 10.1097/LGT.0000000000000525.
- Bonde JH et al. Clinical utility of human papillomavirus genotyping in cervical cancer screening: a systematic review. J Low Genit Tract Dis. 2020;24(1):1-13. doi: 10.1097/LGT.0000000000000494.
- Stoler MH et al. Stratified risk of high-grade cervical disease using onclarity HPV extended genotyping in women, ≥25 years of age, with NILM cytology. Gynecol Oncol. 2019;153(1):26-33. doi: 10.1016/j.ygyno.2018.12.024 .
About the Author

Molly Broache, MSN
Molly Broache, MSN, is Senior Global Medical Science Liaison for Becton, Dickinson and Company (BD) and is also licensed as a women’s health nurse practitioner in both Maryland and Virginia. At BD, Broache focuses on medical and scientific education, training, and engagement for the BD women’s health portfolio of products.