Researchers at Massachusetts General Hospital (MGH), the Dana-Farber Cancer Institute and other Boston-area research centers are turning the tables on glioblastomas, the most devastating and aggressive form of brain cancer, by transforming a type of cell that normally protects tumors and inhibits effective drug therapy into a stone-cold glioblastoma killer, according to a news release from Mass General.
Glioblastoma, a type of brain tumor, is rapidly fatal: Most patients die within two years of diagnosis despite aggressive therapies, such as brain surgery, whole-brain radiation and chemotherapy.
Despite hopes that a class of drugs known as immune checkpoint blockers (ICBs) – drugs that have revolutionized the treatment of patients with malignant melanoma, non-small-cell lung cancer, and other solid tumors – could also benefit patients with glioblastoma, ICBs have not been effective against the disease in clinical trials to date.
ICBs work by removing the brakes on the immune system, allowing previously inactive immune cells to recognize, attack and destroy mutated, cancerous cells while causing minimal damage to the normal tissues.
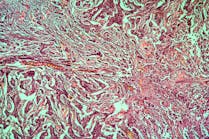
But as Rakesh K. Jain, PhD, Director of the Edwin L. Steele Laboratories in the Department of Radiation Oncology at MGH, and colleagues show in a study published in Nature Communications, glioblastomas wreak havoc with the immune system by altering the landscape surrounding and within the tumor, known as the tumor microenvironment, reorganizing blood vessels, immune cells, and tissue structural proteins into an abnormal glioblastoma-promoting environment, effectively hampering the action of ICBs.
“These abnormalities promote a suppressive environment for the immune system, which blocks tumor-fighting immune cells at the tumor border while allowing infiltration of tumor-promoting immune cells known as regulatory T cells, or Tregs,” explains Jain, who is also Andrew Werk Cook Professor of Radiation Oncology at Harvard Medical School (HMS). “Among elements of the tumor microenvironment, we exploited the preferential accumulation of Tregs in glioblastoma by therapeutically altering their function – a strategy known as reprogramming – to make them kill cancer cells instead of protecting them,” he continues. “Because Tregs already present in these tumors can be reprogrammed, this strategy does not rely on additional recruitment of anti-tumor immune cells – another frequent barrier to successful immunotherapy in brain tumors.”
The investigators accomplished Treg conversions by targeting a receptor (docking site) on glioblastoma Tregs called glucocorticoid-induced TNFR-related receptor (GITR), using an antibody (αGITR) that reprograms the tumor promoter into a tumor-fighting type of T cell.
“In addition to showing that Tregs can be reprogrammed from tumor promoters to cancer killers, our study also demonstrated that a potent anti-tumor effect can be generated by both alleviating Treg-mediated resistance to immunotherapy and by reinvigorating CD8+ T cells, one of the major players in immune responses against cancer,” explains co-corresponding author Hye-Jung Kim, PhD, Immunologist at the Dana-Farber Cancer Institute.
Their findings support the use of αGITR antibodies in combination with ICBs, with or without the current standard-of-care therapies, in patients with glioblastomas who have high levels of Tregs, Jain says.