The absence of a protein that works to prevent tumor formation may explain why some patients are resistant to a common cancer therapy, according to Penn State College of Medicine researchers and reported in a press release. They said that testing cancers for the presence of this protein may help clinicians identify patients who may be resistant to or relapse when treated with the therapy.
Epidermal growth factor receptor (EGFR) is a protein that plays a role in cell division and survival signaling and is active in skin, bladder, esophageal, lung, liver, pancreatic, colon, and head and neck cancers. Patients with high amounts of this protein in their tumors tend to have a poor prognosis. EGFR-targeting therapies are used in clinical practice and are often initially effective in many patients. However, some patients are resistant to the therapy and many who were initially responsive to treatment relapse within a year.
Douglas Stairs, Assistant Professor of Pathology and Laboratory Medicine and Pharmacology, investigated why these patients may be resistant to EGFR therapies. He said mutations in the gene that contains the instructions for building EGFR or other genetic and cellular factors account for about 70 percent of resistance causes.
“There are still some reasons for resistance that are alluding scientists,” said Stairs, a Penn State Cancer Institute researcher. “Our previous work showed that too much EGFR and reduced amounts of a protein called p120 catenin (p120ctn) can cause cancer to develop. We hypothesized that reduced amounts of p120ctn might also cause resistance to EGFR therapies.”
In healthy cells, p120ctn strengthens cell-to-cell contact by cooperating with other proteins to strengthen connections between epithelial cells, which serve as the barrier between the body’s external and internal surfaces. According to Stairs, scientists know that the cancer cells often have reduced amounts of p120ctn but are unsure why.
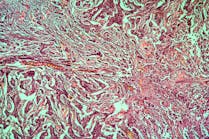
To test their hypothesis, Stairs and colleagues cultured genetically-engineered esophageal cancer cells — one set with normal amounts of EGFR and p120ctn, one set with higher amounts of EGFR, one set with lower amounts of p120ctn and another set with high amounts of EGFR and low amounts of p120ctn. They then treated each cell line with a series of EGFR-targeting therapies.
Cells with high amounts of EGFR died when treated with the therapies, while those with normal amounts of EGFR were not affected by the therapies. The cell lines that had high amounts of EGFR and reduced amounts of p120ctn were resistant — demonstrating that loss of p120ctn is a critical component to the cells’ resistance to EGFR-targeted therapies. The results were published in PLOS ONE.
Stairs said that while these results are promising, his lab will continue to explore the role of p120ctn loss in EGFR therapy resistance by testing the effect in cancer cells sampled from patients with colon, lung, oral or other cancers. They will also explore whether the cells with increased EGFR and decreased p120ctn are resistant to other EGFR therapies approved by the U.S. Food and Drug Administration.
“We also need to investigate further how the loss of p120ctn causes this resistance,” Stairs said. “For now, we know that if patients who have high levels of EGFR in their samples were also tested for their levels of p120ctn, it may provide a clue to clinicians as to which patients are at risk for resistance to EGFR-targeting therapies or relapse.”