Tomography is an imaging technique used across a wide variety of fields, ranging from radiology and nuclear medicine, to geophysics and materials science. It provides three-dimensional information about a subject based on its sections or projections, and common examples include X-ray, computed tomography (CT), positron emission tomography (PET), and single-photon emission computed tomography (SPECT). CT scanning provides information on the anatomy of the subject, while PET provides functional imaging which shows the spatial distribution of biomolecular activity in the body. PET was developed as a technology for both clinical diagnostic and preclinical purposes in the 1950s, the scope of which was expanded by the development of radiopharmaceuticals—a group of pharmaceutical drugs which emit radiation and commonly includes radiotracers.
Preclinical imaging (PCI) plays a vital role in understanding the biological processes behind disease states at the organ, tissue, cell, and molecular level. Elucidating how the body responds to physiological or environmental change is important in the search for therapeutic agents to fight disease. PCI is also critical to the evaluation of new treatment effectiveness and safety, by informing researchers of drug distribution patterns in tissues. PET in preclinical studies enables users to conduct repeat experiments on the same animal subjects, providing strong statistically valuable data and, therefore, reducing the number of animals required for a study. For this reason, it has become increasingly important to use non-invasive in vivo imaging techniques to optimize the use of each animal used. Multi-modal tomographs, such as PET/CT, allow the correlation of the functional imaging obtained using PET with the anatomic imaging obtained with CT scanning. PET can also be combined with other technologies, such as magnetic resonance imaging (MRI), to bring functional imaging together with soft tissue morphological imaging. PET/MR is gaining ground in preclinical imaging applications, as it offers superior soft tissue contrast, imaging without the CT’s ionizing radiation risk, and multiparametric data.
Preclinical PET applications
PET, PET/CT, SPECT/CT, PET/MR, and PET/SPECT/CT multi-modal imaging techniques are used across a number of life science applications, including oncology and neurology. Total body PET imaging is also possible and enables researchers to determine the pharmacokinetics of new drugs in all the body’s organs and tissues at low masses.
Oncology
Preclinical researchers are interested in understanding the biology of tumor development, response to cancer treatment, and drug toxicity. There are various types of tumors, some of which have not yet been well characterized, so imaging technologies such as PET can shed light on the mechanisms of progression for many different tumor types, and how treatment affects them.
Many cancers are associated with a higher metabolic turnover than normal cells so, using PET and an injected radiolabeled glucose analogue tracer such as fluorine-18 (18F)-fludeoxyglucose (18F-FDG), glucose uptake can be quantified and tumor burdens detected. This method can also be used to detect molecular biomarkers to contribute to cancer detection and treatment response assessment. PET/CT and, more recently, PET/MR are used to determine the accumulation regions of 18F-FDG, to obtain a semiquantitative standardized uptake value (SUV) to assist in the diagnosis of tumor malignancy.
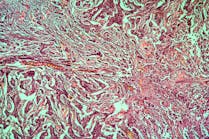
Combination cancer therapies are often desired for their ability to address multiple molecular targets, as well as a reduced chance of drug resistance. A relevant study used preclinical PET/CT imaging to monitor 18F-FDG tumor uptake for different treatment combinations: Radiotherapy (Rad) alone, Rad + Temozolamide (Tmz), Rad + Mifepristone (Mife), and Rad + Mife + Tmz. Rad + Tmz is the typical treatment regime for glioblastoma, but the study found that using Mife as a priming agent suppressed tumor growth more than the other treatment combinations (Figure 1).1 The mechanism of this chemo-radio-sensitizing effect of Mife is yet to be fully characterized, but studies such as this help researchers make important steps toward improving available cancer treatments.
Preclinical laboratories are increasingly aware of the benefits of PET/MR for oncology research. Thanks to MRI’s unique ability for imaging soft tissue, users can visualize the true tumor margin and evaluate tracer distribution within individual tumors to generate a desired volume of interest (VOI) and calculate SUVs more accurately. Tumor margin detection is a unique and significant enhancement to preclinical cancer PET studies.
Neurology
Neuroscientists benefit from PET imaging technologies to obtain metabolic information about the brain, for example to detect changes in brain metabolic activity that might be indicative of abnormalities, potentially leading to conditions such as Alzheimer’s Disease (AD), Parkinson’s Disease (PD), stroke, memory loss, and cognitive decline. PET imaging is also used for the study of addiction and psychiatric disorders. By using PET in preclinical studies on the brain’s impact on behavior and cognition, researchers can advance their understanding about nervous system processes in healthy individuals, in addition to various disease states, and elucidate abnormalities in its organization and connectivity.
PET/MR is particularly useful in neurology as it provides synchronized soft-tissue images with metabolic imaging, enabling scientists to investigate the brain’s anatomical structures, pathologies, and metabolic abnormalities in preclinical animal models. Researchers can use PET and MRI to localize molecular markers in brain tissue, and image brain microstructure, connectivity, vasculature, and activity at high resolution.
Neurodegenerative diseases, such as AD, PD, multiple sclerosis, and Huntington’s disease are a key focus of preclinical research, with MRI technology providing the high spatial resolution in vivo imaging required to determine the structure and function of central nervous system tissues. Used in tandem with MRI, PET imaging enables scientists to investigate the pathological hallmarks of neurodegenerative disease, such as amyloid-β (Aβ) and tau protein depositions in AD models.
Similarly, to oncological applications, glucose metabolism is a useful biomarker for many neurological disorders. Normal brain glucose metabolism is modified by many disease states and can be easily monitored by 18F-FDG-PET. Currently, most AD treatments are targeted toward the disease’s symptoms, rather than the underlying causes. Some studies have investigated the possibility of halting AD progression with therapeutics that target the early stage causes of the disease. For example, one experiment found that a new candidate therapeutic synthetic cannabinoid, JWH, a selective CB2 agonist, significantly increased metabolic activity in the hippocampus and cortical regions of mice, measured by 18F-FDG-PET.2 The mice also showed reduced neuroinflammation and an increase in Aββ clearance when administered with JWH, improving overall cognitive performance.
Advances in PET technology
There are a number of performance criteria that PET systems must meet to provide the highest quality imaging results. Resolution and sensitivity depend, in part, on the material in the detector stopping the gamma rays (the scintillator) and the detector design. A very dense material is needed to stop as many gamma rays as possible. Dense and thick scintillator crystals that convert the gamma energy into light are therefore the material of choice in PET detectors. The size of the crystal impacts PET resolution. Diameter of the ring and depth of interaction (DOI) correction must also be optimized for high-resolution imaging. Crystal technology also underpins PET sensitivity and has undergone a number of advances in recent years. The industry has been dominated by pixelated crystals, tightly packed together, but the use of continuous crystals has shown to better measure light distribution and, therefore, provides greatly improved resolution and sensitivity.
New advanced PET instruments combine continuous crystal scintillators with novel light detection technology for superior imaging capabilities. Rather than using traditional avalanche photodiodes (APD) or photomultiplier tubes (PMTs), continuous crystals are coupled with silicon photomultiplier (SiPM) photosensors to allow the accurate determination of all three spatial coordinates of the gamma photon interaction within the detector crystal. The result is sub millimetric spatial resolution, regardless of the positron, a term known as full field accuracy (FFA). FFA results in more reproducible data, independent of variable sample positioning, and more reliable imaging of large samples or multiple animals across the field of view (FOV), to facilitate accuracy and throughput in preclinical imaging.
Preclinical PET in the future
Multi-modal PET imaging is enabling scientists to break new ground in preclinical research spanning a number of fields. As a highly sensitive, non-invasive technique, PET can help improve the understanding of the underlying causes of disease, improving methods of detection and treatment. Preclinical PET studies facilitate the development of imaging biomarkers, with the goal to translate these to the clinical to identify patients at risk or in the early stages of disease.
REFERENCES
- Llaguno-Munive M, Medina LA, Jurado R, Romero-Piña M, Garcia-Lopez P. 2013. Mifepristone improves chemo-radiation response in glioblastoma xenografts. Cancer Cell International. 13:29. https://doi.org/10.1186/1475-2867-13-29
- Martín-Moreno AM, Brera B, Spuch C, et al. 2012. Prolonged oral cannabinoid administration prevents neuroinflammation, lowers β-amyloid levels and improved cognitive performance in Tg APP 2576 mice. Journal of Neuroinflammation. 9:8. doi:10.1186/1742-2094-9-8.
![Figure 1. PET/CT images showing 18F-FDG tumor uptake, in four treatment combinations, at the beginning of treatment and 25 days later. Red arrows indicate tumor location at baseline and day 25, green arrows show sites of typical 18F-FDG uptake in brown adipose tissue (BAT). Reproduced from reference [1] in accordance with the Creative Commons License (https://creativecommons.org/licenses/by/2.0/). Figure 1. PET/CT images showing 18F-FDG tumor uptake, in four treatment combinations, at the beginning of treatment and 25 days later. Red arrows indicate tumor location at baseline and day 25, green arrows show sites of typical 18F-FDG uptake in brown adipose tissue (BAT). Reproduced from reference [1] in accordance with the Creative Commons License (https://creativecommons.org/licenses/by/2.0/).](https://img.mlo-online.com/files/base/ebm/mlo/image/2019/07/mouse.5d30996e633a1.png?auto=format,compress&fit=max&q=45&w=250&width=250)