SARS-CoV-2 variants evade most – but not all – antibodies
New research indicates that three new, fast-spreading variants of the virus that cause COVID-19 can evade antibodies that work against the original form of the virus that sparked the pandemic. Whether such antibodies were produced in response to vaccination, natural infection, or were purified antibodies used as drugs, researchers found more antibody is needed to neutralize the variants.
However, several highly neutralizing monoclonal antibody cocktails, including those developed at Vanderbilt University Medical Center, showed intact or only mildly diminished activity against the variants tested, possibly because they target sites on the spike protein other than the highly mutable E484K residue.
The findings, from laboratory-based experiments and published in Nature Medicine, suggest that COVID-19 drugs and vaccines developed thus far may become less effective as the new variants become dominant, as experts say they inevitably will. The researchers looked at variants from South Africa (B.1.135), the United Kingdom (B.1.1.7) and Brazil (B.1.1.248, also known as P.1.)
The multi-center research was led by Washington University School of Medicine in St. Louis. In addition to Vanderbilt University Medical Center, University of Texas Medical Branch also participated in the work.
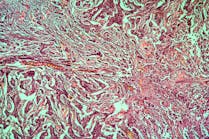
The virus that causes COVID-19, known as SARS-CoV-2, uses a protein called spike to latch onto and get inside cells. Consequently, spike became the prime target for COVID-19 drug and vaccine developers. And potent anti-spike antibodies were selected for development into antibody-based drugs for COVID-19.
The researchers tested the variants against antibodies in the blood of people who had recovered from SARS-CoV-2 infection or were vaccinated with the Pfizer vaccine. They also tested antibodies in the blood of mice, hamsters and monkeys that had been vaccinated with an experimental COVID-19 vaccine, developed at Washington University School of Medicine, that can be given through the nose. The B.1.1.7 (United Kingdom) variant could be neutralized with similar levels of antibodies as were needed to neutralize the original virus. But the other two variants required from 3.5 to 10 times as much antibody for neutralization.
They also tested monoclonal antibodies: mass-produced replicas of individual antibodies that are exceptionally good at neutralizing the original virus. When the researchers tested the new viral variants against a panel of monoclonal antibodies, the results ranged from broadly effective to completely ineffective.
Since each virus variant carried multiple mutations in the spike gene, the researchers created a panel of viruses with single mutations, so they could parse out the effect of each mutation. Most of the variation in antibody effectiveness could be attributed to a single amino acid change in the spike protein. This change, called E484K, was found in the B.1.135 (South Africa) and B.1.1.248 (Brazil) variants, but not B.1.1.7 (U.K.).
CMS addresses CLIA certification violations
As a result of a recent record check, the Centers for Medicare and Medicaid Services (CMS) issued 171 cease-and-desist letters to facilities that did not have proper certifications in place as outlined in the Clinical Laboratory Improvement Amendments of 1988 (CLIA). CLIA certification is important, because it verifies that laboratories meet federal performance, quality and safety standards to properly diagnose, prevent and treat diseases.
CMS said that every facility that conducts COVID-19 testing is considered a “laboratory” and must be certified under CLIA. To make certification easy, CMS implemented an expedited review process at the beginning of the public health emergency and recently released a quick-start guide to help laboratories with the application process. CMS said that it is imperative to public safety that facilities apply for CLIA certification and only operate within the scope of that certification to prevent false results that could adversely alter diagnosis or treatments and contribute to the further spread of COVID-19.
False positive results possible with Roche test
The FDA announced that false positive results can occur with the Roche Molecular Systems cobas SARS-CoV-2 & Influenza A/B Nucleic Acid Test for use on the cobas Liat System.
Roche’s assay tubes may sporadically leak, causing an obstructed optical path in the Liat analyzer, producing abnormal PCR growth curves, leading to invalid or erroneous positive results, particularly for the Flu B test. If a tube leak occurs, later testing runs may have an increased likelihood of false positive Flu B results.
Roche also determined that abnormal PCR cycling in the reaction tubes may produce abnormal PCR growth curves, caused by simultaneous factors, such as hardware positioning, volume movement, and curve interpretation. This issue may cause false positive results for multiple analytes (Influenza A, Influenza B and/or SARS-CoV-2) in a single testing run.
The FDA recommends users of the cobas SARS-CoV-2 & Influenza A/B Nucleic Acid Test for use on the cobas Liat System:
- Watch out for unexpected clusters of positive Flu B results, as this may indicate the cobas Liat System has experienced a tube leak.
- Repeat tests when two or three analytes are positive. Different results on the repeat test may indicate abnormal PCR cycling.
- Stop using the cobas Liat System and contact Roche if you suspect either of these two issues has occurred.
NIH scientists develop breath test for methylmalonic acidemia
Researchers at the National Institutes of Health (NIH) have developed a breath test that measures how well patients with methylmalonic acidemia (MMA) respond to receiving liver and/or kidney transplantation. Researchers used the test to assess the severity of the disease in people and help determine if they would benefit from surgical or experimental genomic therapies that target the liver.
MMA is a rare genomic disease that impairs the body’s ability to metabolize certain proteins and fats. This causes toxic build up, causing kidney disease, pancreatitis, movement disorders, intellectual impairments, organ complications, or, in severe cases, death. Currently, MMA is incurable, and some patients receive liver and/or kidney transplants to help restore normal levels of metabolic proteins.
One form of MMA is caused by mutations in the methylmalonyl-CoA mutase gene (MMUT), which encodes for the MMUT protein. People with this form of MMA have a deficiency in the MMUT protein, which plays a pivotal part in metabolism by breaking down food, fats, cholesterol and amino acids.
MMUT helps break down food into a chemical byproduct called propionate, which is followed by oxidation, where a healthy body converts propionate into energy and carbon dioxide, which is exhaled, but that process is faulty for people with MMA.
Because MMUT protein function is compromised in people with MMA, the team chose to assess how well the MMUT protein helped break down propionate in both patients who did and not did not receive treatment.
To detect if the MMUT protein was functioning properly, researchers gave patients a dose of the heavier, less abundant version of carbon – carbon 13 – via a commercially available food additive.
The team recruited 57 study participants, including 19 MMA patients who had received transplants (liver, kidney or both) and 16 healthy volunteers. Researchers gave participants a dose of the food additive containing carbon 13 via a drink or through a feeding tube, and then collected their breath samples after a two-minute wait.
The researchers measured how much of the exhaled carbon dioxide contained the usual carbon 12 compared to added carbon 13. MMA patients who did not receive any treatment had lower levels of carbon 13 than healthy volunteers. By contrast, MMA patients with liver transplants had higher levels of carbon 13, similar to the healthy volunteers.
FDA updates on COVID-19 testing
The U.S. Food and Drug Administration (FDA) recently granted emergency use authorization (EUA) for numerous COVID-19 tests.
These include the Quidel QuickVue At-Home OTC COVID-19 test for OTC at-home serial screening; Abbott BinaxNOW COVID-19 Antigen Self Test for OTC at-home serial screening; Abbott BinaxNOW COVID-19 Ag Card 2 Home Test for OTC at-home serial screening with telehealth; Abbott BinaxNOW COVID-19 Ag 2 Card for POC serial screening without a prescription; BD Veritor System for Rapid Detection of SARS-CoV-2 for POC serial screening with a prescription; and the Symbiotica COVID-19 Self-Collected Antibody Test System, which is the first antibody test authorized for use with home collected dried blood spot samples.
The FDA also warned that false positive results can occur with antigen tests to detect SARS-CoV-2, particularly when users do not follow the instructions, including routine follow-up testing (reflex testing) with a molecular assay when appropriate, and by considering the expected occurrence of false positive results when interpreting test results.
When using antigen tests, the FDA said to follow instructions in the package insert about handling test cartridges/cards, such as ensuring they are not stored open, and reading test results at the appropriate time. Use caution when processing multiple specimens in batch mode because the process may make it challenging to ensure the correct incubation time for each specimen. Minimize the risks of cross-contamination when testing patient specimens, which can cause false positive results.
As the impact of SARS-CoV-2 variants on diagnostic test results is another issue facing laboratories, the FDA created a new web page: SARS-CoV-2 Viral Mutations: Impact on COVID-19 Tests | FDA.
The FDA revised an announcement regarding the doses per vial available for the Moderna COVID-19 vaccine.
The FDA first clarifies the maximum extractable doses per vial is 11, with a range of 10-11 doses. In the second revision, the agency authorized the use of an additional multi-dose vial that contains a maximum of 15 doses, with a range of 13-15 doses that can potentially be extracted.
Depending on the type of syringes and needles used to extract each dose, there may not be sufficient volume to extract more than 10 doses from the vial containing a maximum of 11 doses or more than 13 doses from the vial containing a maximum of 15 doses.
Because the Moderna COVID-19 vaccine does not contain preservatives, any further remaining product that does not constitute a full dose should not be pooled from multiple vials to create one full dose. If one vial becomes contaminated during use, pooling doses from multiple vials can spread contamination to other vials.