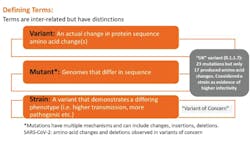
SARS-CoV-2 is the RNA coronavirus responsible for the COVID-19 global pandemic. Just when newly approved vaccines (and many more in development) offered the prospect of a return to normalcy, the emergence of highly circulating variants has raised significant concerns about vaccine efficacy.1-3 The term “viral variant” can be confusing and is often (and incorrectly) used interchangeably with other terms, such as mutations, strains, and lineages.1 Figure 1 describes formal definitions and distinctions. Mutations are normal, abundant, and expected, especially with an RNA virus. When a mutation or group of mutations confers an advantage, a new variant can emerge. If the altered phenotype allows it to outcompete existing virus (for example, if it is more infectious or more capable of evading immune pressure), it may become the dominant strain.
Variants have been with us since the beginning
As confirmed by the recent joint investigation by the World Health Organization (WHO) and Chinese scientific teams, variants have been with us since the dawn of the pandemic.4 It was a presumed variant that produced one or more strains highly capable of infecting humans (likely from a yet-to-be-identified zoonotic progenitor that may trace back to bats), principally through changes in the spike protein that increased viral affinity for the human ACE2 receptor. The original “Wuhan” strain was subsequently displaced outside China by a variant with a single amino acid change at position 614 in the S1 region of spike protein that changed an aspartic acid to a glycine (D614G).5-7 Starting in April of 2020, D614G spread rapidly to become the dominant global strain. Data indicates the D614G variant has increased infectiousness, but fortunately, it remains susceptible to current vaccines based on the original Wuhan strain.
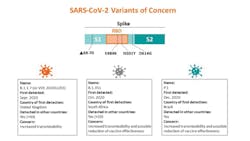
New “variants of concern”
Despite the rapid spread of D614G as the dominant strain, until recently, much of the public remained unaware of variants. The identification of “variants of concern” (VOC) in several parts of the world (including those first identified in the United Kingdom, South Africa, Brazil, and the United States, but now detected in multiple countries) has elevated recognition and prompted investigation.1-3 More variants continue to be identified globally, as countries initiate enhanced sequence surveillance programs, with the greatest focus on mutations in the spike protein. Concerns include impairment of some diagnostic tests, including a small subset of molecular tests where the mutation impacts primer annealing, or the possibility of changes that enhance pathogenesis or transmission.
The United States has recently identified a commonly emerging variant with a mutation in S2 (Q677P) that may enhance fusion of virus with the host cell.8 An additional variant spreading rapidly in California has a mutation in spike at position 452 (L452R) that has also sparked concerns of potential increased transmission and possible resistance to a neutralizing antibody.9 The variant first identified in the United Kingdom (B.1.1.7) shares a mutation with the variants first noted in Brazil and South Africa at position 501 (N501Y) that may increase transmission. B.1.1.7 is present in the United States, and some predict it will become a dominant variant, as it appears to be spreading rapidly.10 Though not yet determined, worries also exist on increased pathogenicity with B.1.1.7. Of significant concern with any spike/RBD mutants is the potential for resistance to, or escape from, neutralizing antibodies from recovered infection or, more relevantly, vaccination.
Vaccines target the spike protein
All currently approved vaccines (and most in development) target the viral spike protein, which contains the receptor-binding domain (RBD) that recognizes and binds the virus to the ACE2 receptor on the host cell.11 Therefore, a spike or RBD-based assay must be used if assessing a vaccine antibody response if the nucleoprotein is not a part of the construct. Abundant data show the RBD is the primary target of neutralizing antibodies.12-14 Since neutralizing antibodies can interfere with viral binding and so limit infection, they are especially appealing as a mechanism of inducing protection.
Vaccine study data using whole spike show highly correlated detection of binding and neutralizing antibodies using either spike or RBD-based assays (unsurprising, as the RBD is contained in the spike).15-17 “Neutralizing” antibodies are defined by their ability to inhibit infection in-vitro, which often translates to protection in-vivo. Vaccine-related data generated with animal models has clearly established the importance of spike/RBD antibodies for protection from SARS-CoV-2 challenge.18,19 Thus, changes in the RBD are of particular concern, though mutations in the S1-NTD and S2 may also present a potential immune escape adaptation.
Role for neutralizing antibodies
While data indicate that elements of both the cellular (T-cell) and humoral (B-cells producing antibody) adaptive immune response contribute to protection from (re)infection, neutralizing antibody alone has been shown to be highly significant.19-21 Therapies based on neutralizing antibodies are utilized and include both monoclonal-based and convalescent plasma (CP).
Importantly, the level of neutralizing antibodies may be essential for vaccine efficacy and therapeutic CP. Vaccines requiring a two-dose regimen resulted from observations that a single dose failed to achieve sufficient seroconversion and titer of neutralizing antibody. While vaccine-induced antibody responses may generally be higher compared to many recovered infections, levels vary between subjects. The current unknown is if individual susceptibility for infection (including variants) is associated with variable neutralizing antibody levels in vaccine recipients. Infusion of highly neutralizing polyclonal serum in animal models subsequently challenged with live virus indicate a protective threshold exists and may be important for protection.19
RBD mutations and immune escape
To better understand worries for variants able to evade/resist neutralizing antibody, an understanding of the current mutations of concern is required. Figure 2 shows some of the the mutations of concern in spike protien.22 Mutations can include an amino acid coding change, a deletion, or an insertion. Most mutations are either silent or eliminated as deleterious, but a subset may improve viral fitness. Mutations occur throughout the viral genome but not with equal frequency. “Hotspots” exist and include the spike protein.23 While some RBD variants have shown the ability to resist/evade some neutralizing antibody, other mutations in spike may also contribute to evasion. These include deletions in the S1 N-terminal domain and mutations in S2 also found in these variants.8,24,25
Selective pressure and immune escape variants
One significant potential source of environmental selective pressure is the presence of neutralizing antibodies. In tissue culture, SARS-CoV-2 rapidly mutates with passage in the presence of neutralizing antibody, developing resistance that necessitates higher titers of antibody to neutralize.26 The variable resistance observed for variants and individual CP samples may result from the types of neutralizing antibodies arising from the polyclonal response or high versus lower antibody levels.27,28
Vaccines may be in a race with variants, as lack of widespread protection may promote increased pressure for selection of resistance. Variants better able to evade antibody neutralization may exploit this vulnerability and become the dominant strain (especially if also more transmissible), potentially challenging successful vaccination efforts.29
The need to modify current vaccines and variants
It will be essential to understand if escape variants translate to increased susceptivity in vaccinated populations. Despite a reduction in neutralization in-vitro, relevant protection in a vaccinated individual may remain, especially if neutralizing antibodies are high or if elements of T-cell immunity are able to compensate. Alternatively, “variant specific” vaccine boosts may be important. Vaccine trial data from regions of high variant transmission do indicate a reduction (but not elimination) in current vaccine efficacy with variants (though primarily limited to analysis showing symptomatic clinical infection). For example, preliminary vaccine trial results for a recombinant spike protein-based vaccine showed 89 percent efficacy in the United Kingdom (including B.1.1.7 infections), but a reduced efficacy of 49 percent in South Africa, where the B.1.351 (also called 501Y.V2) variant with three RBD mutations predominates.30
Early data (requiring additional confirmation) from a chimp adenoviral-based vaccine trial, also conducted in South Africa, showed essentially no difference in rates of mild to moderate infection in the vaccinated population.31 However, data for the same vaccine in the United Kingdom indicates it is effective at limiting infection and that a higher efficacy was observed even with the B1.1.7 variant, including significant protection from a single dose.32 The ability to reduce severe disease or hospitalization may be an important parameter, even with impaired efficacy, as shown in data from a similar vaccine using a human adenoviral vector also encoding the spike protein.33
While the format of the vaccine (e.g., mRNA, adenoviral, recombinant protein etc.) may be a factor impacting efficacy, it will be necessary functionally to understand the role levels of neutralizing antibodies and cellular immune components play following vaccination. Data points to the level of neutralizing antibody, much of it targeted to the RBD, as a major component of protection.12-14,19 Quantitative testing for antibody targeted to known neutralizing regions like RBD or whole-spike assays is likely salient for assessment of protection, including with variants.The same variant can arise independently
Some mutations or groups of mutations are shared between distinct variants, so they likely confer an advantage. Parallel evolution in independently arising variants is almost certain and supported by genome analysis.9,23,24 Therefore, the finding of the “UK” variant in multiple countries may trace back to imported cases or arose from local mutagenesis. With enhanced surveillance, a better understanding of variant emergence and frequency will evolve. Consistent findings of recurrent mutations indicate lockdowns on international travel may be insufficient to control variant spread.
A mutation at position 501 (N501Y) in the RBD is shared by the three highly reported strains and has been linked to potentially higher receptor affinity and increased infectiousness.22 Two additional mutated positions in the RBD are shared by the South Africa (B.1.351) and Brazil (P.1) strains (K417T, E484K). The E484K mutation alone has been linked with both reinfection and reductions in neutralization from both CP and some vaccine sera.28,34,35
However, encouraging in-vitro data has been published for vaccine sera from recipients of the currently approved mRNA vaccines. Comparatively small reductions in neutralization were observed with sera from individuals who’d received both doses of the BNT162b2 vaccine when tested with several spike mutations found in the three highly circulating variants.36 In similar data, sera from recipients receiving both doses of mRNA-1273 vaccine showed generally modest reductions in neutralization; although, constructs with the three RBD mutations alone or for all mutations identified in B.1.351 did reveal notable reductions in, but not elimination, of neutralization.37
The N501Y mutation (shared by the 3 common variants and the only RBD mutation found in B1.1.7) appears to remain largely susceptible to vaccine-induced neutralizing antibodies. Importantly, studies thus far examining these various mutations have used primarily pseudoviral constructs representing either a subset or the constellation of mutations associated with a given variant. While this data is highly useful, testing with live virus variants will be necessary to confirm findings.38
(Semi)quantitative testing for spike or RBD antibody following vaccination
As variants emerge and spread, it will be essential to understand if there is a continued role for the level or titer of neutralizing antibody induced against a prior strain (such as the Wuhan strain spike sequence used by several vaccines) and protection from a new variant.14,28,39 Studies with CP and variants suggest that the level of neutralizing antibody may indeed matter, as CP with high levels of neutralizing antibody appears to offer greater protection against mutated strains.28 Data indicating continued if diminshed protection from some spike mutations in vaccinated individuals is encouraging, but also suggests the level of neutralizing antibody may be a significant factor if higher levels are required to maintain protection.40
What is essential to know is if (semi)quantitative tests might show a significant reduction in reported value with antibodies associated with spike variants. While levels of spike/RBD antibodies are most salient to neutralization, testing for seroprevalence or evidence of infection can utilize either spike or nucleocapsid antibodies. Since mutations can impact both the nucleocapsid and spike proteins, all assays are potentially susceptible based on the antigenic regions they target.
At least some manufacturers are working to determine this with their respective assays, although initial limitations in variant-infection sample access present a challenge. While the polyclonal nature of the response would suggest continued detection (as assays detect antibody to multiple epitopes), the possibility of a reduced signal or need for a “variant specific” threshold exists. Further investigation is needed to elucidate this.
Aiding the simplified assessment for the level of antibody (versus titer) is the increasing availability of quantitative SARS-CoV-2 antibody assays (technically semi-quantitative in the United States, due to the current lack of an accepted international reference standard). Moreover, some manufacturers have published correlation data to specific neutralization titers determined by plaque reduction neutralization assay (PRNT), which uses live virus in the presence of differing levels of antibody to assess for percent inhibition of viral infection in cell culture and is considered the gold standard neutralization method. Such assays could support studies with dominant viral variant infections to assess for any altered “variant threshold” that may be associated with protection relative to the prior strain. Thresholds could have clinical implications as to protection/vulnerability and inform decisions of need to boost or prioritize for variant-specific vaccines should they become available.Are “variant-specific” vaccines required immediately?
It is clear from the vaccine trial data to date that sterilizing immunity is unlikely to be achieved with vaccination. Vaccinations may be more aligned with preventing severe disease or hospitalizations. The limited data to date with approved vaccines indicates a level of protection may persist with the variants, albeit at reduced levels.35-38 This likely reflects the polyclonal nature of the neutralizing antibody, elements of cellular immunity, and variability in individual vaccine responses.
There is intriguing data using sera from patients recovered from COVID-19 and given a single dose of an approved mRNA vaccine, showing an almost thousand-fold increase in the ability to neutralize the highly-mutated B.1.351 variant, which supports continued utility with at least some available vaccines.40 The authors determined that antibodies to the RBD were a primary source of neutralization (with some contribution from antibodies in S2) and that increased vaccine-induced levels may be essential for effective neutralization. Therefore, immediate modification of existing vaccines may not be exigent (though may be important for optimal protection overall), at least in individuals with high levels of spike/RBD antibodies.
The FDA and “high-titer” CP: immunoassay values correlate
The recent emergency use authorization (EUA) issuance from the U.S. Food and Drug Administration (FDA) of validated assay-specific cut-points for SARS-CoV-2 screening of “high-titer” CP further indicates a role for neutralizing antibody level.41 If given early, high-titer CP appears therapeutic and may mitigate disease, presumably by interfering with the ability of the virus to bind to or fuse with the host cell. Since wide variability is seen for neutralizing antibodies with CP, it is critical to identify high titer for use as a therapeutic, as low-titer plasma does not perform well. This FDA issuance of correlated values vastly simplifies the identification of acceptable CP donations and supports the value of (semi)quantitative antibody testing.
Conclusion
Variants of concern will continue to emerge, and enhanced surveillance will support earlier identification. Currently, data indicates that at least with most available vaccines, protection is maintained, albeit at a reduced level in some. It is unknown if new viable variants with additional spike mutations will emerge, or what further impact they might have on vaccination. Spike/RDB-based semi-quantitative antibody tests could prove highly useful, especially if levels of antibody post-vaccination are confirmed as a relevent correlate of protection for circulating virus, including variants.
References:
- Lauring AS, Hodcroft EB. Genetic variants of SARS-CoV-2—What do they mean? JAMA. 2021;325(6):529-531. doi: 10.1001/jama.2020.27124.
- Fontanet A, Autran B, Lina B, et al. SARS-CoV-2 variants and ending the COVID-19 pandemic. Lancet. 2021. doi: 10.1016/s0140-6736(21)00370-6.
- Mascola JR, Graham BS, Fauci AS. SARS-CoV-2 viral variants—tackling a moving target. JAMA. 2021. doi: 10.1001/jama.2021.2088.
- Mathers M. Wuhan already had 13 variants of Covid by December 2019, WHO team finds. The Independent. Published February 15, 2021. https://www.independent.co.uk/news/world/asia/wuhan-covid-variants-december-2019-who-investigation-b1802393.html. Accessed March 1, 2021.
- Hou YJ, Chiba S, Halfmann P, et al. SARS-CoV-2 D614G variant exhibits enhanced replication ex vivo and earlier transmission in vivo. Science. 2020;370(6523):1464-1468. doi: 10.1126/science.abe8499.
- Yurkovetskiy L, Wang X, Pascal KE, et al. Structural and functional analysis of the D614G SARS-CoV-2 spike protein variant. Cell. 2020;183:739–751. doi: 10.1016/j.cell.2020.09.032.
- Plante JA, Liu Y, Liu J, et al. Spike mutation D614G alters SARS-CoV-2 fitness. Nature. 2020. doi: 10.1038/s41586-020-2895-3.
- Hodcroft EB. Emergence in late 2020 of multiple lineages of SARS-CoV-2 spike protein variants affecting amino acid position 677. medRxiv. 2021. doi: 10.1101/2021.02.12.21251658.
- Li Q, Wu J, Nie J, et al. The impact of mutations in SARS-CoV-2 spike on viral infectivity and antigenicity. Cell. 2020;182(5):1284–1294. doi:10.1016/j.cell.2020.07.012.
- Galloway SE, Paul P, MacCannell DR, et al. Emergence of SARS-CoV-2 B.1.1.7 lineage – United States, December 29, 2020–January 12, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:95–99. doi: 10.15585/mmwr.mm7003e2.
- Krammer, F. SARS-CoV-2 vaccines in development. Nature. 2020;586:516–527. doi: 10.1038/s41586-020-2798-3.
- Piccoli L, Park Y-J, Tortorici MA, et al. Mapping neutralizing and immunodominant sites on the SARS-CoV-2 spike receptor-binding domain by structure-guided high-resolution serology. Cell. 2020;183(4):1024-1042. doi: 10.1016/j.cell.2020.09.037.
- Premkumar L, Segovia-Chumbez B, Jadi R, et al. The receptor binding domain of the viral spike protein is an immunodominant and highly specific target of antibodies in SARS-CoV-2 patients. Sci Immunol. 2020;5(48). doi:10.1126/sciimmunol.abc8413.
- Wajnberg A, Amanat F, Firpo A, et al. Robust neutralizing antibodies to SARS-CoV-2 infection persist for months. Science. 2020;370(6521):1227-1230. doi: 10.1126/science.abd7728.
- Jackson LA, Anderson EJ, Rouphael NG, et al. An mRNA Vaccine against SARS-CoV-2 —Preliminary Report. N Engl J Med. 2020;383:1920-31. doi: 10.1056/NEJMoa2022483.
- Mulligan MJ, Lyke KE, Kitchin N, et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature. 2020;586(7830):589-593. doi: 10.1038/s41586-020-2639-4.
- Walsh EE, Frenck Jr. RW, Falsey AR, et al. Safety and immunogenicity of two RNA-based Covid-19 vaccine candidates. N Engl J Med. 2020;383(25):2439-2450. doi: 10.1056/NEJMoa2027906.
- Corbett KS, Flynn B, Foulds KE, et al. Evaluation of the mRNA-1273 vaccine against SARS-CoV-2 in nonhuman primates. N Engl J Med. 2020;383:1544-1555. doi: 10.1056/NEJMoa2024671.
- McMahan K, Yu J, Mercado NB, et al. Correlates of protection against SARS-CoV-2 in rhesus macaques. Nature. 2021;590:630-634. doi: 10.1038/s41586-020-03041-6.
- Dan JM, Mateus J, Kato Y, et al. Immunological memory to SARS-CoV-2 assessed for up to 8 months after infection. Science. 2021;371(6529). doi: 10.1126/science.abf4063.
- Stephens DS, McElrath MJ. COVID-19 and the path to immunity. JAMA. 2020;324(13):1279–1281. doi: 10.1001/jama.2020.16656.
- Centers for Disease Control and Prevention. Emerging SARS-CoV-2 variants. CDC. February 11, 2020. Updated January 28, 2021. https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/scientific-brief-emerging-variants.html. Accessed March 1, 2021.
- Laamarti M, Alouane T, Kartti S, et al. Large scale genomic analysis of 3067 SARS-CoV-2 genomes reveals a clonal geo-distribution and a rich genetic variations of hotspots mutations. PLoS ONE. 2020;15(11). doi: 10.1371/journal.pone.0240345.
- McCarthy KR, Rennick LJ, Nambulli S, et al. Recurrent deletions in the SARS-CoV-2 spike glycoprotein drive antibody escape. Science. 2021 Feb 3;eabf6950. doi:10.1126/science.abf6950.
- Kemp SA, Collier DA, Datir R, et al. Neutralising antibodies in Spike mediated SARS-CoV-2 adaptation. medRxiv.2020. doi: 10.1101/2020.12.05.20241927.
- Greaney AJ, Starr TN, Gilchuk P, et al. Complete mapping of mutations to the SARS-CoV-2 spike receptor-binding domain that escape antibody recognition. Cell Host Microbe. 2021;29(1):44-57. doi: 10.1016/j.chom.2020.11.007.
- Wang P, Nair MS, Liu L, et al. Increased resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7 to antibody neutralization. bioRxiv. 2021. doi: 10.1101/2021.01.25.428137.
- Wibmer CK, Ayres F, Hermanus T, et al. SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. bioRxiv. 2021. doi: 10.1101/2021.01.18.427166.
- Williams TC, Burger WA. SARS-CoV-2 evolution and vaccines: cause for concern? Lancet Respir Med. 2021. doi: 10.1016/S2213-2600(21)00075-8.
- Novavax. COVID-19 vaccine demonstrates 89.3% efficacy in UK phase 3 trial: first to demonstrate clinical efficacy against COVID-19 and both UK and South Africa variants. Novavax. January 28, 2021. https://ir.novavax.com/node/15506/pdf. Accessed March 3, 2021.
- Mueller B, Robbins R, Chutel L. AstraZeneca’s vaccine does not work well against virus variant in South Africa. The New York Times. February 7, 2021. https://www.nytimes.com/2021/02/07/world/africa/covid-vaccine-astrazeneca-south-africa.html. Accessed February 17, 2021.
- Voysey M, Clemens SAC, Madhi SA, et al. Single dose administration, and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine. Lancet. February 1, 2021. https://ssrn.com/abstract=3777268.
- Johnson & Johnson announces single-shot Janssen COVID-19 vaccine candidate met primary endpoints in interim analysis of its phase 3 ENSEMBLE trial. Janssen. January 29, 2021. https://www.janssen.com/johnson-johnson-announces-single-shot-janssen-covid-19-vaccine-candidate-met-primary-endpoints. Accessed March 3, 2021.
- Resende PC, Bezerra JF, Teixeira de Vasconcelos RH, et al. Spike E484K mutation in the first SARS-CoV-2 reinfection case confirmed in Brazil, 2020. https://virological.org/t/spike-e484k-mutation-in-the-first-sars-cov-2-reinfection-case-confirmed-in-brazil-2020/584. Accessed Feb. 17, 2021.
- Collier DA, De Marco A, Ferreira IATM, et al. SARS-CoV-2 B.1.1.7 escape from mRNA vaccine-elicited neutralizing antibodies. medRxiv. 2021. https://www.medrxiv.org/content/10.1101/2021.01.19.21249840v2?versioned=true.
- Xie X, Liu Y, Liu J, et al. Neutralization of SARS-CoV-2 spike 69/70 deletion, E484K and N501Y variants by BNT162b2 vaccine-elicited sera. Nat Med. 2021. doi: 10.1038/s41591-021-01270-4.
- Wu K, Werner AP, Koch M, et al. Serum neutralizing activity elicited by mRNA-1273 vaccine — preliminary report. N Engl J Med. 2021. doi:10.1056/NEJMc2102179.
- Wu K, Werner AP, Moliva JI, et al. mRNA-1273 vaccine induces neutralizing antibodies against spike mutants from global SARS-CoV-2 variants. bioRxiv. 2021. doi: 10.1101/2021.01.25.427948.
- Gundlapalli AV, Salerno RM, Brooks JT, et al. CDC COVID-19 response, SARS-CoV-2 serologic assay needs for the next phase of the US COVID-19 pandemic response. Open Forum Infect Dis. 2021;8(1). doi: 10.1093/ofid/ofaa555.
- Stamatatos L, Czartoski J, Wan Y-H, et al. Antibodies elicited by SARS-CoV-2 infection and boosted by vaccination neutralize an emerging variant and SARS-CoV-1. medRxiv. 2021. https://doi.org/10.1101/2021.02.05.21251182.
- FDA. Convalescent plasma EUA letter of authorization. Food and Drug Administration. https://www.fda.gov/media/141477/download. Accessed Feb. 17, 2021.