Reimbursement for laboratory services – Are you leaving money on the table?
The traditional view of the total testing process (TTP) consists of pre-analytic, analytic, and post-analytic phases. However, one must also consider a post-post-analytic phase — the process needed to get paid. Understanding the reimbursement process can mean whether a laboratory is profitable or a money loser. Medical billing is complex with many opportunities for denials and rejections. In the United States, 15%-17% of medical private payor claims are initially denied.1,2 It has been reported that up to 80% of medical bills contain errors amounting to $68 billion annually. There are many sources for errors including chronic staffing shortages, from clinician burnout to support staff shortages, all contributing to payment denials.3,4 Laboratory managers must understand billing practices, for failure to do so can significantly impact a laboratory’s revenue stream.
What laboratory managers need to know
The players
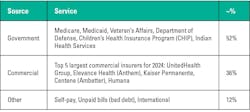
There are over 1,100 third-party health insurance payors in the United States, all with different reimbursement plans and requirements. Knowing who the third-party payors are (payor mix) sets the playing field for understanding the rules in how charges are submitted and reimbursed. Table 1 lists the payor mix.
CPT and ICD codes®
Every laboratory has a chargemaster — a list of all laboratory tests by CPT code (Current Procedural Terminology) that is updated annually. In addition, ICD-10 codes (International Classification of Diseases, 10th revision) are also used to identify specific medical diagnoses/procedures. ICD-10 codes are currently used in the United States, however, ICD-11 codes were approved and released in 2022 by the WHO and adopted by more than sixty countries. The United States’ transition to ICD-11 will occur between 2025 and 2027.
Denials and what to do with them?
Up to 65% of medical billing claims are not reworked resulting in a 20% to 30% loss in revenue.5 The laboratory is a high-volume service with many more CPT codes than other healthcare services thus greater opportunities for errors can occur. Further, reworking denied payments for services such as MRIs, surgeries, etc. often takes priority over less expensive laboratory tests.2
CPT issues
The following are a few procedural errors that may occur in up to 45% of charges due to the misuse or omission of a CPT code. Note: Attempting to enhance reimbursements by manipulating CPT codes is a compliance issue.6
- Modifiers are codes appended to CPT codes indicating additional information about a service is available. Table 2a lists some common modifiers used for laboratory services. Improper use of modifiers may account for 8% of billing errors.
- Duplicate billing occurs when the same test/service is billed twice. If a repeat test is medically necessary, a modifier is required. (13% of errors)
- Unbundling is when the components of a panel are billed separately. Table 2b is an example of unbundling an electrolyte panel that incorrectly enhances reimbursements. (10% of billing errors)
- Upcoding occurs when a more complex and expensive CPT code is used when a less complex and cheaper test was actually performed (15% of billing errors). Table 2c illustrates how a qualitative test was performed but charged as a quantitative test getting a higher reimbursement.
ICD coding issues
ICD coding requires communication between the healthcare provider and the laboratory. A submitted ICD code must medically support why a specific test was ordered, i.e., medical necessity. Up to 60% of medical bills may be in error due to improper diagnosis codes (ICD codes).
- Non-FDA-approved tests, experimental tests, and screening tests are generally not covered and will be denied unless an Advanced Beneficiary Notice (ABN) is obtained. Example: modified or non-commercially available kits used to test for glucose or protein tests on body fluids.
- Laboratory tests that are not explicitly covered by a third-party payor will require a pre-authorization. Many molecular and genetic tests fall into this category.7
- National Correct Coding Initiative (NCCI) edits were developed by Medicare to promote appropriate coding methodologies and minimize improper billing submissions. Though mainly used by Medicare, many insurance companies use similar edits. The following are some key components.
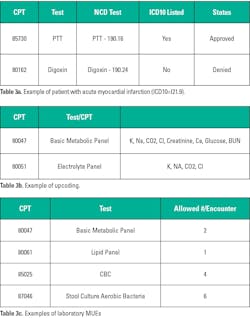
- NCDs (National Coverage Determinations): There are twenty-three policies covering some common tests, listing the CPT code(s) and the acceptable ICD codes. The claim will be denied if the ICD code is not on the list. Table 3a shows an example of a patient with acute myocardial infarction (ICD10= I21.9) who had two tests performed: PTT and Digoxin.
- PTP (Procedure to Procedure Edits) identifies certain tests (CPT) that cannot be billed at the same patient encounter. Table 3b shows two panels that cannot be ordered/performed at the same patient encounter. Generally, the least expensive of the two will be reimbursed.
- MUE (Mutually Unlikely Edits) identifies the maximum number of times a specific test can be ordered during the same date of service. Table 3c shows a few examples.
- LCDs (Local Coverage Determinations) supplement NCDs in covering medically necessary items or services that are managed locally and vary from location to location. Similar to MUEs, some LCD policies may further define the frequency of testing, e.g., lipids, thyroid testing, glucose testing, or glycated hemoglobin.
- Laboratories using outdated or deleted ICD codes will result in a denial. Of note, ICD-11 contains four times more codes than ICD-10, thus opening up opportunities for miscoding.
Other sources of error
- Typographic errors or omissions account for 27% of denials.5 Examples include misspelled names, common surnames (Smith, Jones, etc.), and generational designations (II, III, Jr., Sr.) that can be easily confused. Wrong birthdates, dates of service, or insurance numbers are also major sources of errors. Failure to notify a change of address or last name (due to marital status) will also lead to a denial.
- Change in employment often means a change in healthcare plans, thus a patient needs to ensure that they submit the correct insurance to their provider. Patients seeking healthcare services from a non-participating provider (out-of-network provider) will receive a denial of payment.1
- Timely filing is dictated by an insurance company specifying the period within which a claim must be received, and if not, will be denied (6% of errors). Timely filing cutoffs vary by payor ranging from 90 days to a year. Denied charges that are not promptly worked and resubmitted can miss the deadline especially when payors are slow to respond (up to 60 days) with a denial.8
- Place of Service (POS) — these two-digit codes are required on the claim forms to indicate where the patient was at the time of service, i.e., hospitals, clinics, emergency facilities, hospices, etc. (4% of errors). If a patient is transferred from a nursing facility (POS 31) to a hospital (POS 21) and the POS was not changed, all hospital services will be denied.6
Appeals
Denials interrupt laboratory cash flow and if not followed up promptly can be a significant loss of revenue. It has been reported that up to 60% of returned claims were not corrected and resubmitted, yet two-thirds of these denials are appealable. Denials take time to review and investigate as to why they were denied/rejected. The average cost to initially file a claim correctly is less than $7, while the cost to review and fix a denial ranges from $25 to over $100. Submitting a clean claim is the goal.5,9 Often, charges for a denied claim are passed on to the patient with almost 44% having problems paying their medical bills; 64% of these specifically had problems paying for laboratory services.10
Conclusion
Laboratory managers must educate themselves about laboratory billing and take the lead in resolving and fixing denial problems. Failure to do so leads to loss of revenue and potential compliance concerns. CPT codes are updated annually and ICD codes in April and October of each year. Purchasing CPT and ICD manuals can help laboratory managers identify coding changes. Errors in Medicare/Medicaid billing, whether accidental or intentional, can result in an audit, the consequences of which can include repayment, penalties, criminal charges, and exclusion from all federally funded programs. Government-based insurance can account for as much as 50% of a laboratory’s revenue. Understanding Medicare/Medicaid rules is critical since they serve as a model for commercial payors. Knowing the payor mix and reimbursement rates allows a manager to focus on the best and highest payors and can play an important part in developing an annual budget. Looking at the reimbursement rates for the top 25 high-volume tests by payor is a good start in ensuring correct billing practices. Review the chargemaster for current CPT codes. Any recent price increases in reagents, equipment, controls, salaries, or overhead should be reflected in assessing charges by performing a test cost analysis (TCA) if needed, especially for the more complex, time-consuming, or expensive tests such as genetic, molecular, and mass spectrometry assays.11
Contacting the laboratory’s billing agent to find out denial claim statistics and routinely reviewing them can help identify trends or other systemic problems, whether it’s a personnel problem or software issue. Proactively train and educate personnel in billing procedures. A bi-directional relationship with the billing department can educate billers about unique differences in laboratory procedures and conversely, educate laboratorians about billing rules and regulations. Also developing a relationship with office personnel from high-volume clinics/providers can be useful in obtaining diagnosis and pre-authorization information. Ensuring the phlebotomy staff collects the right/correct information at the time of service can eliminate potential errors.
Finally, commercial insurance companies have used rule-based artificial intelligence (AI) algorithms and machine learning to sort claims and initiate denials. It has been noted that some algorithms fail to evaluate claims accurately, thus improperly initiating denials. Some laboratories have integrated AI with their laboratory information system (LIS), which can manage various functions including time-consuming repetitive tasks, processing of claims, and flagging errors before they are released. AI uses past denial experiences to predict future denial issues. However, even with the aid of AI, it is still necessary to perform regular internal audits to ensure billing practices are accurate and legal, thus minimizing denials, improving cash flow, and reducing potential compliance issues.3,8,12
References
1. Pollitz K, Lo J, Wallace R, Mengistu S. Claims denials and appeals in ACA Marketplace plans in 2021. KFF. February 9, 2023. Accessed November 20, 2024. https://www.kff.org/private-insurance/issue-brief/claims-denials-and-appeals-in-aca-marketplace-plans/.
2. Trend alert: Private payers retain profits by refusing or delaying legitimate medical claims. Premier. March 21, 2024. Accessed November 20, 2024. https://premierinc.com/newsroom/blog/trend-alert-private-payers-retain-profits-by-refusing-or-delaying-legitimate-medical-claims.
3. Leveraging AI and automation to minimize claim denials in healthcare. Experian Health. Published August 1, 2024. Accessed November 20, 2024. https://www.experian.com/blogs/healthcare/prevent-claim-denials-with-ai-and-automation/#.
4. Moneypenny M. Over 20 woeful medical billing error statistics — etactics. Etactics | Revenue Cycle Software. October 20, 2020. Accessed November 20, 2024. https://etactics.com/blog/medical-billing-error-statistics.
5. Reduce denials and increase your lab’s revenue and net collections. Ligolab. September 23, 2024. Accessed November 20, 2024. https://www.ligolab.com/post/reduce-denials-and-increase-your-labs-revenue-and-net-collections.
6. Lindner J. Study reveals shocking medical billing errors statistics impacting Americans. Gitnux. July 17, 2024. Accessed November 20, 2024. https://gitnux.org/medical-billing-errors-statistics/.
7. Bonislawski A. Prior authorization a growing headache for labs as payors clamp down on molecular, genetic testing. 360Dx. May 16, 2024. Accessed November 20, 2024. https://www.360dx.com/clinical-lab-management/prior-authorization-growing-headache-labs-payors-clamp-down-molecular.
8. Williams J. Battle of the Bots: As payers use AI to drive denials higher, providers fight back. HFMA. March 28, 2024. Accessed November 20, 2024. https://www.hfma.org/revenue-cycle/denials-management/health-systems-start-to-fight-back-against-ai-powered-robots-driving-denial-rates-higher/.
9. Poland L, Harihara S. Claims denials: A step-by-step approach to resolution. J AMIHA. April 25, 2022. Accessed November 20, 2024. https://journal.ahima.org/page/claims-denials-a-step-by-step-approach-to-resolution.
10. Hamel L, Norton M, Pollitz K, Levitt L, Claxton G, Brodie M. The burden of medical debt: Results from the Kaiser Family Foundation/New York times medical bills survey. KFF. January 5, 2016. Accessed November 20, 2024. https://www.kff.org/health-costs/report/the-burden-of-medical-debt-results-from-the-kaiser-family-foundationnew-york-times-medical-bills-survey/view/print/.
11. WHO Laboratory test costing tool. (World Health Organization; 2019). Published 2019. Accessed November 20, 2024. https://iris.who.int/bitstream/handle/10665/346135/WHO-EURO-2019-3484-43243-60604-eng.pdf?sequence=3.
12. Mello MM, Rose S. Denial—artificial intelligence tools and health insurance coverage decisions. JAMA Health Forum. 2024;5(3):e240622. doi:10.1001/jamahealthforum.2024.0622.
13. Emerson J. Payer mix in the nation’s largest for-profit health systems. August 9, 2023. Accessed November 20, 2024. https://www.beckershospitalreview.com/hospital-finance/payer-mix-in-the-nations-largest-for-profit-health-systems.html.
14. Novitas. Modifiers. Novitas Solutions. Updated April 17, 2023. Accessed November 20, 2024. https://www.novitas-solutions.com/webcenter/portal/MedicareJH/pagebyid?contentId=00003604.
About the Author

Anthony Kurec, MS, MASCP, MLT, H(ASCP)DLM
is Clinical Associate Professor, Emeritus, at SUNY Upstate Medical University in Syracuse, NY. He is also a member of the MLO Editorial Advisory Board.