Best practices for reducing unnecessary preoperative blood orders and associated costs
Every day, anesthesiologists and surgeons consider the appropriate preoperative blood product order for each patient entering the operating room. Blood product ordering includes obtaining either ABO group blood typing and red cell antibody screening (T/S) or a type and crossmatch for a specific number of units (T/C). A surgery with a low probability of transfusion does not require a blood product order, while other procedures may require just a T/S or additionally a T/C. Appropriate ordering is imperative to ensure that resources are directed to process samples and prepare products for cases with a likelihood of hemorrhage and transfusion and also to minimize costs associated with unnecessary testing.
MSBOS
A Maximum Surgical Blood Order Schedule (MSBOS) includes guidelines for preoperative blood product ordering and was first described in 1976 by Friedman.1 A MSBOS should ideally be institution- and procedure-specific, based on blood utilization data. In 2013, our team used data from our electronic Anesthesia Information Management System (AIMS) to analyze blood utilization data from more than 53,000 patients undergoing 135 categories of surgical procedures at our institution and ultimately developed an algorithm for deriving an institution-specific MSBOS.2 Our MSBOS includes a list of cases for which a preoperative blood order is unnecessary based on our institutional rate of transfusion. The backup plan for unexpected transfusions in such patients without blood orders is the use of type O red cells for emergency release, which is much safer than most providers acknowledge. With the implementation of our MSBOS, we hypothesized that our institution would see a reduction in unnecessary blood orders and thus associated cost savings.
EBRS
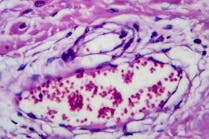
Simultaneous with the release of our MSBOS we implemented another major advance in transfusion medicine: the remote electronic blood release system (EBRS). The EBRS functions as a “vending machine” for red blood cell (RBC) units, which is located within each operating room suite and electronically linked to the blood bank. The EBRS relies on an electronic crossmatch, which is performed in seconds just before the RBC unit is dispensed. The electronic crossmatch has been performed at our institution for over 10 years and can be used for any patient without red cell antibodies if his or her ABO group has been typed at least twice in the hospital’s system. This is accomplished on a validated computer system with software to screen for discrepancies and match ABO-group specific compatible blood. Since the electronic crossmatch can be performed immediately before the transfusion, it promotes more efficient blood-ordering practices.
One measure of the efficiency of blood-ordering and transfusion practices is the crossmatch-to-transfusion (C/T) ratio. This ratio analyzes the total number of cross-matched red cell units in relation to the actual number of units transfused. A high C/T ratio implies that unnecessary crossmatches were performed when a type and screen or no order at all would have been more appropriate. Today a benchmark of transfusion practice is a C/T ratio of 2.0 or lower.
Measuring the effect
With the simultaneous release of our MSBOS and rollout of the EBRS we studied the effect of these two interventions on our blood-ordering and transfusion processes.3 We hypothesized that these measures would result in more efficient transfusion practices as measured by the C/T ratio as well as decreased unnecessary blood orders and costs. Using our institution’s AIMS data, we analyzed 63,916 patients who had undergone a surgical procedure (after excluding pediatric, obstetric, endoscopy, and ophthalmology cases) between January 2011 and October 2013. Our updated MSBOS and our EBRS were implemented in July 2012. We also used an additional transfusion database to assess the C/T ratio for all hospitalized inpatients (n = 136,640) in our institution over the same time period, as not all patients had undergone a procedure where AIMS data would be available but providers did receive education on the electronic crossmatch.
In surgical patients undergoing procedures in the MSBOS “no sample needed” category, the percent with any blood order decreased by 38.1% in the post-MSBOS/ERBS period (from 40.4% to 25.5%; P<0.001). When examining data from all hospitalized inpatients, the C/T ratio decreased by 27.1% from 2.11 to 1.54 (P<0.001), bringing the ratio below the 2.0 benchmark. Cost analysis was performed by using the number of surgical patients with a T/S or T/C ordered and the 2013 Medicare reimbursement rates, and our institution saw a decrease in annual costs by $137,223 ($6.08 per patient) in the post-MSBOS/ERBS period. For all inpatients, we assessed the annualized cost of crossmatches according to the C/T ratios before and after the MSBOS/ERBS release and found a decrease in cost of $298,966 per year ($6.20 per patient).
We did see a small increase in the transfusion of uncrossmatched emergency release blood in the post-MSBOS/ERBS time period from 0.22% to 0.31% of patients. Over the 34-month period of our study, 162 patients required emergency release blood, with 98 of those (60%) having emergency surgery. In the MSBOS “no sample needed” category, there was a small increase in emergency release blood transfusion from 0.4 in 1,000 patients to 1 in 1,000 patients. There were no ABO incompatibility hemolytic reactions, and we are unaware of any minor or delayed hemolytic reactions from these emergency release transfusions.
Positive outcomes
In summary, at our institution, we have implemented both an updated MSBOS with clinician education and an ERBS and found that our rates of unnecessary blood orders, our C/T ratio, and associated costs decreased. We did see a small but clinically insignificant increase in the transfusion of emergency release blood products following these measures. Clinicians today must focus on reducing both unnecessary testing and cost without compromising patient safety. In this era, our findings have particular relevance and contribute to standardizing care and providing quality metrics.
REFERENCES
- Friedman BA. An analysis of surgical blood use in United States hospitals with application to the maximum surgical blood order schedule. Transfusion. 1979;19(3):268-278.
- Frank SM, Rothschild JA, Masear CG, et al. Optimizing preoperative blood ordering with data acquired from an anesthesia information management system. Anesthesiology. 2013;118(6):1286-1297.
- Frank SM, Oleyar MJ, Ness PM, Tobian AR. Reducing unnecessary preoperative blood orders and costs by implementing an updated institution-specific maximum surgical blood order schedule and a remote electronic blood release system. Anesthesiology. 2014;121(3):501-509.
Conflicts of Interests and Sources of Funding Dr. Frank has received funding from Haemonetics (Braintree, MA), Zimmer-Biomet (Warsaw, IN), Medtronic (Minneapolis, MN). All other authors have no conflicts to declare.
Courtney G. Masear, MD, is an Assistant Professor in the Department of Anesthesiology and Critical Care Medicine at the Johns Hopkins University School of Medicine. Her clinical subspecialty is obstetric anesthesiology, and her research interests include intraoperative blood utilization and anesthesiology resident education.
Steven M. Frank, MD, is an Associate Professor at the Johns Hopkins Medical Institutions. His clinical expertise is in anesthesia for patients undergoing vascular, thoracic, and transplant surgical procedures. He is Director of the Interdisciplinary Blood Management Program and Medical Director of the Center for Bloodless Medicine and Surgery at Johns Hopkins.