For years, it has been common practice in many hospitals for phlebotomy to draw extra blood tubes in the emergency department (ED) “just in case.”1 Also, ED nurses often collect an array of tubes when they start IVs “just in case” the specimens might be needed for further testing. There is a perception that ED patients will typically require additional or follow-up testing, so drawing these extra tubes prevents the need for a second blood draw. Phlebotomy and ED nursing staff not only believe they are saving patients this second “poke” but that they are saving themselves time by drawing the blood in advance. Thus, when laboratory phlebotomists receive an order for testing, they end up drawing a rainbow of extra colored tubes during the initial blood draw.
The laboratory staff at a large hospital system in the Midwest noticed that their process for managing a high volume of extra blood tubes drawn from patients during ED visits, without physician orders, was bogging down the specimen reception department. An Internet and a library search did not find any documented studies supporting the clinical need for drawing these extra blood tubes, or a discussion of real benefits to the patient. This led to a series of questions. How many extra tubes were arriving in the laboratory? How many were actually used? Were these extra tubes necessary for excellent patient care?
Process analysis and results
The initial project for our team was to develop or improve the existing process for managing extra tubes coming into the laboratory from the ED. Historically, this process had been very cumbersome for our laboratory specimen receiving department (Figure 1). For example, since the extra tubes were not ordered via the hospital’s computer system, a bar-coded label was not automatically printed and available for these tubes. In fact, extra tubes were not completely documented until our reception area intervened. Tubes without physician orders were set aside until our laboratory staff had time to create an order in the system and add a bar-coded label to the tube. If there were no additional orders within the first couple of hours of receipt, we would move the tubes onto the automated line, mapping them and placing them in appropriate racks for storage.
When we analyzed our process, we discovered that our specimen reception department was taking 1.75 minutes per tube to manage the extra tubes that were not ordered in the system. With an average of 400 tubes per day, this work equaled almost 12 person hours/day, 7 days a week. In addition, our analysis found that only 16 of the 400 extra tubes drawn (4%) were used for testing. We also found we could normally use specimens already in the laboratory for add-on testing requested by the physicians.
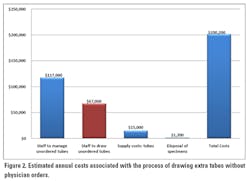
Our team also evaluated costs to the laboratory for the management of the extra tubes drawn in the ED. Figure 2 shows a breakdown of this cost analysis, with annual costs based on an average of 400 extra tubes drawn per day. The costs to the laboratory were estimated to be $200,200 annually. The high cost of the system included the time staff spent drawing the tubes—40% nursing, 60% phlebotomy—and time spent managing the tubes throughout the process—50% technologist, 50% laboratory specimen receptionist.We then questioned the value of these costs to patient care. Our team members agreed to evaluate the value of drawing extra tubes in the ED by developing a report that would flag the extra tubes drawn and identify which ones were utilized in the laboratory for add-on orders by the ED physicians.
Changes in practice
As we looked further at the data to understand the common practice of drawing extra tubes, we quickly discovered that, at 4% utilization, the extra tubes had very low value to the staff and patients. Further analysis showed that either additional testing was added to the original tube or the physician wanted a fresh tube drawn for an update on the patient’s current status. It is important to note that we did not look at the process and data for extra tubes drawn as part of the orderable for a trauma set. These tubes were physician-ordered and were already properly labeled and available in the laboratory for add-on testing as ordered.
Following a presentation to staff about our analysis of the existing process and low value of drawing extra tubes, our ED leaders and laboratory leaders agreed that the extra draws were a waste of resources, generating unnecessary costs. Representatives from phlebotomy and ED nursing met to discuss a proposal: to no longer draw extra tubes in the ED without physician orders. Everyone seemed surprised when they saw our analysis. They believed the extra tubes were being used for add-on testing and that they were saving patients a second “poke.” They also believed they were saving time for themselves by not having to go back for a second draw. However, our data showed that staff were actually spending more time drawing extra tubes than was being saved because a second draw was seldom necessary.
Both clinical areas (i.e., phlebotomy and ED nursing) agreed to discontinue drawing extra tubes unless ordered by the physician. The clinical staff felt that there were times a physician would want extra tubes available. So we worked with the hospital’s computer systems department to add a new orderable called “Extra Tube-Rainbow Set.” This set prints out the appropriate labels and tells the clinical person drawing blood which tubes have been ordered by the physician. Since these tubes are properly ordered and labeled, there is no extra management in the laboratory reception area, and the tubes are placed on the automated line for processing. If no specific testing order has been received prior to the tubes being set on the line, the automated line maps the specimens into a rack for future retrieval as add-on testing is requested.
Outcomes
When we implemented the new process, there was an immediate drop from 400 tubes per day drawn without orders to zero extra tubes per day drawn without orders. A three-month check of the data still showed full compliance, with no extra tubes being drawn without physician orders. The number of extra tubes ordered by physicians also was reduced from 75 per day to 45 per day as they realized there was a very limited need for drawing extra tubes.
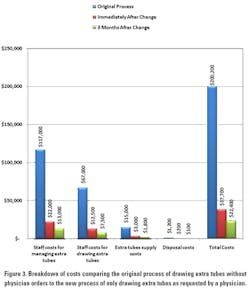
Significant cost savings in our laboratory were realized immediately after the process was changed. The cost savings were broken down into four categories: staffing time to manage the extra tubes; staffing time to draw and handle the extra tubes; supply costs; and the cost to dispose of the extra tubes. As Figure 3 shows, after the process had been in place for 90 days, the estimated saving was more than $200,000 annually. The cost reductions came from staff reassignments, a reduction in staff time to draw extra tubes, and reductions in overall supply costs and specimen disposal costs. Although we might not see the cost savings from staff reassignments reflected directly in the bottom line, we have been growing 5% to 6% per year. The reassigned staff now work in areas that would have required an increase in FTEs, resulting in an overall cost saving for the laboratory.
Conclusion
Laboratories will continue to see testing volume increase and reimbursement decrease. To cope with these trends, laboratory managers need to further increase the efficiency of staff by eliminating waste in their processes and by identifying processes that are not adding true value to patient care. This includes processes that are considered “traditional.”
Drawing extra tubes in the ED is common practice throughout the United States. Clinicians, with all good intentions, believe they are reducing the number of pokes per patient by drawing extra tubes during the first draw. However, by analyzing the actual use of extra tubes drawn in our ED and conducting a true cost analysis, we found that this process was archaic in our healthcare environment. The challenge now is to identify other traditional processes that are occurring in healthcare today that truly do not add value to patient care—only costs.
Reference
- BloodBankTalk, United States, Transfusion Services forum. Collection of extra tubes-allowed? Where to hold and who? http://www.pathlabtalk.com/forum/showthread.php?1942-collection-of-extra-tubes-allowed-where-to-hold-and-who. Accessed January 16, 2012.