Venous thromboembolism (VTE) is a major health concern in the Western world, occurring in a wide variety of diseases and causing significant mortality and morbidity. The most common manifestations of VTE are deep vein thrombosis (DVT) and pulmonary embolism (PE).1 DVT is a venous thrombotic clot in the lower extremities, the most serious being in the proximal veins and the less serious in calf veins. When a portion of the thrombus breaks loose and lodges in the pulmonary arteries, this results in a pulmonary embolism (PE), the most common fatal aspect of VTE. Most VTE is treatable, reducing morbidity and mortality. The diagnosis of VTE is first a subjective or a clinical impression; this is followed by more objective, albeit expensive, tests.1 However, if not diagnosed, many VTEs become fatal.Currently, objective evaluation (imaging or radiography) for DVT or PE is pursued only after the healthcare provider has a clinical suspicion of VTE. The wide gap between the subjective, clinical impression and the objective, expensive imaging leads to an expensive evaluation of many patients without VTE. If an inexpensive test were utilized to eliminate some of the patients without VTE, significant savings in healthcare costs would result.The D-dimer assay is an inexpensive laboratory test that now exists for the exclusion of VTE. This article will briefly summarize how the D-dimer assay is used and how the cutoff value is established in the clinical lab. Fibrin formation, fibrin breakdownThe D-dimer is a specific fragment of the fibrin clot, requiring three hemostatic stages to be activated for its formation: clot formation (coagulation), cross-linking by Factor XIII, and clot breakdown (fibrinolysis) of fibrin
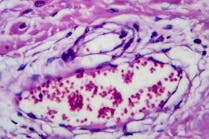
(Figure 1). All three of these steps require the formation of an adequate amount of thrombin. First, thrombin is generated to form the fibrin clot, stopping blood loss. The amount and rate of thrombin and fibrin clot formation are dependent on the coagulation system. Second, thrombin activates Factor XIII, which forms covalent bonds between the clots fibrin molecules
(Figure 2). Finally, the fibrinolytic system, to some extent, requires thrombin in the activation and regulation of plasmin formation
(Figure 3). Plasmin breaks down the fibrin clot into specific, recognizable structural components containing the
D-dimer. Fibrinogen is a large, trilobular, fibrous structural protein that has a linear, three-dimensional shape consisting of two ends (termed D domain) that are identical, with a middle lobe (termed E domain) containing the thrombin activation site. Upon removal of activation peptides, the fibrin monomers self-polymerize when the concentration is critical; the product is termed a fibrin polymer. The assembly of the fibrin monomer is specific wherein two D domains from different fibrin monomers bind to the E domain, forming a linear polymer (Figure 3). Activated Factor XIII forms a covalent link between the two associated D domains. With activation of the fibrinolytic system, the fibrin clot breaks down, thus generating fibrin degradation products containing
D-dimers. These D-dimer-containing fragments circulate in plasma.Diagnosis of venous thromboembolism (DVT and PE)The current clinical procedures for the diagnosis of DVT and PE involve two clinical components.1,2The first is a subjective clinical assessment for probable or suspected DVT or PE. These impressions are based on the history and physical examination of the patient. The second evaluation, utilizing imaging or radiographic methods, is objective, but costly and time-consuming. The gold standard for the diagnosis of DVT is the invasive method of venography, but probably the most commonly used method today is compression ultrasound.1 For PE, the standard imaging method is the ventilation-perfusion scan, but newer methods include spiral CT scans.3,4 Significant disadvantages of most radiographic diagnostic methods include the fact that they are costly, time-consuming, not available 24 hours a day, require special personnel, and, in some cases, have somewhat poor sensitivity.1-4Rationale for use of the
D-dimerDecreasing the use of expensive, time-consuming, and potentially risky procedures to diagnose VTE is a very important goal for todays cost-conscious healthcare system.1,3,5 Plasma markers of hemostasis may help to reduce the use of these procedures. Several markers have been proposed, and the only helpful one to date is the quantitative
D-dimer; however, D-dimer can be used only to rule out VTE, not to confirm VTE.1,6-9 The D-dimers are generated when the fibrin clot is formed, cross-linked, and then degraded.The D-dimer assay is used in several diagnostic venues. Semiquantitative assays help confirm ongoing systemic coagulation seen in disseminated intravascular coagulation (DIC), since DIC usually has very elevated D-dimer levels.10 Quantitative assays are used to exclude DVT and PE. Semiquantitative methods used for DIC must not be used to differentiate the presence or absence of VTE.6,10 Some of the commercial quantitative methods for D-dimer have increased detection range and can be adapted for diagnosis of VTE and DIC, however.3,5-7 The quantitative D-dimer assay can be used only to rule out DVT or PE; in other words, as a negative predictor. If the level of D-dimer in the plasma or blood is not elevated, then no thrombotic process is ongoing, and VTE is not present. However, if the D-dimer level is elevated, a clotting process is occurring, which may be due to VTE, but also may be due to other clinical conditions. Numerous diseases and clinical procedures can increase plasma D-dimer levels without the presence of VTE
(Table 1).Table 1:
Partial list of non-VTE causes of elevated D-dimerDICPregnancyTraumaCancerPost-surgeryDiabetesHematomaThrombolytic therapyArterial thrombosisOlder ageGeneralized hospitalized patientThe rationale for the use of the
D-dimer as a negative predictor is that the formation of a thrombus requires both coagulation and fibrinolytic activation. D-dimer forms only with the activation of the coagulation system (fibrin formation) and the subsequent dissolution of the cross-linked fibrin clot.1,10 Breakdown products of the fibrin clot circulate in the blood and can be detected with monoclonal antibodies specific to D-dimer fragments. The presence of D-dimers suggests that a coagulation-fibrinolytic process is taking place, but does not necessarily confirm that a thrombus has formed.10Clinical assays for
D-dimerSince D-dimers form during a thrombotic process and in numerous other conditions, the D-dimer assay can be used to eliminate the presence of VTE. The assay must be sensitive and specific in the range for differentiation between the presence and absence of a thrombus. Therefore, the cutoff value must be established to exclude all patients with VTE, but not necessarily to include all patients without a thrombus.The D-dimer assay has been established utilizing three different methodologies. All three rely on monoclonal antibodies.5-7,9 The original assay was semiquantitative, utilizing visual macroscopic latex agglutination (used for diagnosis of DIC).10 The most sensitive quantitative D-dimer assays were based on the ELISA format, but are too time-consuming and require specialized equipment and training. The most practical method is based on the concept of microscopic latex agglutination. These assays based on light scattering are usually performed on coagulation instruments, eliminating special equipment needs, but still retaining the needed sensitivity.6-8Unfortunately, all three methods, and even any given method, may produce different results.3-8 These inherent problems occur due to differing monoclonal antibodies, lack of standard calibrators or standards, and inconsistent reporting units. As an example, the designations for reporting units are different and they have different values: 1 Fibrinogen Equivalence Unit (FEU) is approximately equal to 2 D-dimer units.The assay methodology is critical for its practical use in the clinical laboratory or in an outpatient-emergency department setting. Values spanning the cutoff must be accurate and sensitive. The assay must be inexpensive, available 24 hours a day, have a rapid turnaround time, and be performed on routine equipment. If it will be used in a setting other than a clinical laboratory, it must be able to be performed by nonlaboratory personnel.Several preanalytical and analytical variables, as with any coagulation test, may affect the D-dimer assay. Preanalytical variables, such as collection and storage conditions, are the same as for the other routine coagulation tests (PT and aPTT). Analytical variables affecting the quantitative D-dimer again are similar to the routine coagulation and chemistry tests, such as color and turbidity interference. These methodological artifacts must be recognized and corrected.Developing laboratory guidelines
for D-dimer assaysThe most practical commercial D-dimer assays to exclude VTE are based on microscopic latex agglutination using monoclonal antibodies. These antibodies have slightly different affinities and epitopes. Kits are developed specifically for a specific instrument. Therefore, the choice of test method is usually not based on the monoclonal antibody, but on the instrument available to the laboratory; i.e., the choice is based on instrumentation rather than sensitivity and specificity. Most methods have the capability of good negative-predictive value. If a choice of method and instrumentation is an option, then a review of the numerous comparison studies in the current literature should be made. This article does not deal with specific kits, but refers the reader to the literature.Most of the available assays can be automated and are relatively easy to set up and validate. The difficult aspect of establishing the D-dimer assay for exclusion of VTE is establishing the cutoff value. Each laboratory must establish its own cutoff value and cannot rely on a manufacturers recommended value or another laboratorys value. In addition, if the method is set up in the main laboratory and at an off-site location, then the cutoff value must be established for each instrument. The main criterion for establishing the cutoff value is that it must have 100 percent negative-predictive value
(Figure 4). Usually this value is low, near the average of the normal reference range. (The procedure for establishing the cutoff value is outlined in Table
2.) The important concept that cannot be overemphasized is establishing a 100 percent negative prediction that will exclude all individuals with thrombosis. After the initial conservative cutoff has been established, then re-evaluation periodically must be performed by a lookback comparison between D-dimer levels imaging data.
of the D-dimerOnce the D-dimer assay has been validated with an established cutoff level, the assay can be used as a negative predictor for VTE. Guidelines for the use of the D-dimer should be developed with input from clinical staff to develop criteria for its use as a negative predictor.1,2,7 (The guidelines outlined in Table 3 will bring about significant cost savings.) During evaluation of the patient, the clinician categorizes the VTE risk into low, moderate, or high probability. Based on this clinical classification, subsequent testing is ordered. If the patient is classified as low or moderate probability, then a stat. D-dimer test is ordered. If the D-dimer level is above the cutoff value, then imaging procedures are performed. If those are positive, the patient is treated. However, if the D-dimer is below the cutoff value, then VTE is ruled out and other causes are investigated. The patient is not sent to imaging studies nor treated with anticoagulants. Patients with a high probability for VTE should be analyzed by imaging studies and
D-dimer testing bypassed. If positive for VTE, then appropriate anticoagulation therapy is given. If the imaging testing is negative, then other causes are investigated. In all negative cases in which the problem is not identified and persists for five to seven days, or becomes worse, then imaging analysis should be repeated.Table 3:
Clinical models for evaluation of suspected VTELow probability of
VTE:Clinically determined to be low probability by healthcare provider.Stat.
D-dimer assay.If D-dimer is positive (above cutoff),
then perform imaging studies.If imaging studies are positive, treat with anticoagulation.If imaging studies are negative, patient is evaluated for other causes.If D-dimer is negative (below cutoff),
no VTE. No imaging studies are performed.Patient is evaluated for other causes.If symptoms are not identified and persist, re-evaluate in 5 to 7 days.Moderate probability of
VTE:Clinically determined to be moderate probability by healthcare provider.Stat. D-dimer assay.If D-dimer is positive (above cutoff),
then perform imaging studies.If imaging studies are positive, treat with anticoagulation.If imaging studies are negative, patient is evaluated for other causes.If D-dimer is negative (below cutoff),
no VTE. No imaging studies are performed.Patient is evaluated for other causes.If symptoms are not identified and persist, re-evaluate in 5 to 7 days.High probability of
VTE:Clinically determined to be high probability by healthcare provider.Immediate imaging studies and no stat. D-dimer assay.If imaging studies are positive, treat with anticoagulation.If imaging studies are negativeNo VTE.Patient is evaluated for other causes.If symptoms are not identified and persist, re-evaluate in 5 to 7 days.Two major caveats must be incorporated into the procedure for the D-dimer assay: The D-dimer should be used with caution in hospitalized patients, since numerous disease processes and invasive procedures can elevate D-dimer levels without the presence of VTE. In these patients, reliance on clinical evaluation and imaging studies is more valuable.5,6,9 The D-dimer assay should not be used in patients on anticoagulant therapy (heparin or warfarin). Studies have demonstrated that anticoagulants
decrease circulating D-dimers and could possibility generate a false value below the cutoff, and VTE would be missed. It is not recommended that anticoagulated patients be tested for
D-dimer. Most hospitals which utilize the
D-dimer assay for VTE also use the D-dimer assay for confirmation of DIC. Since the range of detection necessary for the two assays is significantly different, we recommend that the hospital provide two assays and offer them as different tests for clinician ordering. In our hospital, we have both tests available; however, they are ordered as different tests with different values and ranges. We differentiate the two assays in the following way: Test name for ruling out VTE is D-dimer (Thrombosis), and the test name for DIC is D-dimer
(DIC).SummaryPatients with venous thrombosis (DVT or PE) have elevated D-dimer, a breakdown product of cross-linked fibrin. The determination of D-dimer levels is both a diagnostic and a cost savings tool to rule out VTE. The assay can be used to eliminate those individuals without VTE, but with low or moderate clinical suspicion. The D-dimer assay is inexpensive, automated, has a rapid turnaround time, and uses standard blue-top tubes. After appropriate validation, the assay can be 100 percent sensitive in ruling out DVT or PE, but it will not confirm the presence of VTE as numerous other diseases and procedures can increase levels. The assay should not be used routinely on inpatients or surgery patients. Caution should be used when interpreting results from patients on anticoagulation therapy, since lower D-dimer levels may be found. If properly used, the
D-dimer assay can save a healthcare facility significant money by eliminating imaging studies on patients with low or moderate suspicion of DVT or PE. Richard A. Marlar is director of the Routine and Special Coagulation Laboratories, Pathology and Laboratory Medicine, at the Denver Veterans Administration Medical Center, and associate professor in the department of pathology, University of Colorado Health Sciences Center, Denver.AcknowledgementsThe author would like to thank Susan Priem and the other personnel of the Denver VA Medical Centers Special Coagulation Laboratory for helping with these studies. This work was supported in part by a A Merit Review Grant and in part by Pathology Service of the Denver VA Medical Center.References1. Anderson DR, Wells PS. D-dimer for the diagnosis of venous thromboembolism. Curr Op Hematol. 2000;7:296-301.2. Janes S, Ashford N. Use of a simplified clinical scoring system and D-dimer testing can reduce the requirements for radiology in the exclusion of deep vein thrombosis by over 20%. Br J Haematol. 2001;112:1079-1082.3. Adams FG. The role of spiral computed tomography and D-dimer in pulmonary embolism. Scott Med J. 2001;46:7-8.4. Righini M, de Moerloose P, Reber G, et al. Should the D-dimer cut off value be increased in elderly patients suspected of pulmonary embolism? Thromb
Haemost. 2001;85:744.5. Anderson DR, Wells PS, Stiell I, et al. Management of patients with suspected deep vein thrombosis in the emergency department: combining use of a clinical diagnosis model with D-dimer testing.
J Emerg Med. 2000;19:225-230.6. Gosselin RC, Owings JT, Utter GH, et al. A new method for measuring D-dimer using immunoturbidity: a study of 255 patients with suspected PE and DVT. Blood Coag
Fibrinolys. 2000;11:715-721.7. Shitrit D, Heyd J, Raveh D, Rudensky B. Diagnostic value of the D-dimer test in deep vein thrombosis: improved results by a new assay and by using discriminate levels. Thromb Res. 2001;102:125-131.8. van der Graaf F, van den Borne H, van der Kolk, et al. Exclusion of deep vein thrombosis with D-dimer testing. Thromb
Haemost. 2000;83:191-198.9. Funfsinn N, Caliezi C, Dermarmels F, et al. Rapid
D-dimer testing and pre-test clinical probability in the exclusion of deep vein thrombosis in symptomatic outpatients. Blood Coag
Fibrinolys. 2001;12:165-170.10. Carey MJ, Rodgers GM. Disseminated intravascular coagulation: clinical and laboratory aspects. Am J Hematol. 1998;59:65-73.©
2002 Nelson Publishing, Inc. All rights reserved.
(Figure 1). All three of these steps require the formation of an adequate amount of thrombin. First, thrombin is generated to form the fibrin clot, stopping blood loss. The amount and rate of thrombin and fibrin clot formation are dependent on the coagulation system. Second, thrombin activates Factor XIII, which forms covalent bonds between the clots fibrin molecules
(Figure 2). Finally, the fibrinolytic system, to some extent, requires thrombin in the activation and regulation of plasmin formation
(Figure 3). Plasmin breaks down the fibrin clot into specific, recognizable structural components containing the
D-dimer. Fibrinogen is a large, trilobular, fibrous structural protein that has a linear, three-dimensional shape consisting of two ends (termed D domain) that are identical, with a middle lobe (termed E domain) containing the thrombin activation site. Upon removal of activation peptides, the fibrin monomers self-polymerize when the concentration is critical; the product is termed a fibrin polymer. The assembly of the fibrin monomer is specific wherein two D domains from different fibrin monomers bind to the E domain, forming a linear polymer (Figure 3). Activated Factor XIII forms a covalent link between the two associated D domains. With activation of the fibrinolytic system, the fibrin clot breaks down, thus generating fibrin degradation products containing
D-dimers. These D-dimer-containing fragments circulate in plasma.Diagnosis of venous thromboembolism (DVT and PE)The current clinical procedures for the diagnosis of DVT and PE involve two clinical components.1,2The first is a subjective clinical assessment for probable or suspected DVT or PE. These impressions are based on the history and physical examination of the patient. The second evaluation, utilizing imaging or radiographic methods, is objective, but costly and time-consuming. The gold standard for the diagnosis of DVT is the invasive method of venography, but probably the most commonly used method today is compression ultrasound.1 For PE, the standard imaging method is the ventilation-perfusion scan, but newer methods include spiral CT scans.3,4 Significant disadvantages of most radiographic diagnostic methods include the fact that they are costly, time-consuming, not available 24 hours a day, require special personnel, and, in some cases, have somewhat poor sensitivity.1-4Rationale for use of the
D-dimerDecreasing the use of expensive, time-consuming, and potentially risky procedures to diagnose VTE is a very important goal for todays cost-conscious healthcare system.1,3,5 Plasma markers of hemostasis may help to reduce the use of these procedures. Several markers have been proposed, and the only helpful one to date is the quantitative
D-dimer; however, D-dimer can be used only to rule out VTE, not to confirm VTE.1,6-9 The D-dimers are generated when the fibrin clot is formed, cross-linked, and then degraded.The D-dimer assay is used in several diagnostic venues. Semiquantitative assays help confirm ongoing systemic coagulation seen in disseminated intravascular coagulation (DIC), since DIC usually has very elevated D-dimer levels.10 Quantitative assays are used to exclude DVT and PE. Semiquantitative methods used for DIC must not be used to differentiate the presence or absence of VTE.6,10 Some of the commercial quantitative methods for D-dimer have increased detection range and can be adapted for diagnosis of VTE and DIC, however.3,5-7 The quantitative D-dimer assay can be used only to rule out DVT or PE; in other words, as a negative predictor. If the level of D-dimer in the plasma or blood is not elevated, then no thrombotic process is ongoing, and VTE is not present. However, if the D-dimer level is elevated, a clotting process is occurring, which may be due to VTE, but also may be due to other clinical conditions. Numerous diseases and clinical procedures can increase plasma D-dimer levels without the presence of VTE
(Table 1).Table 1:
Partial list of non-VTE causes of elevated D-dimerDICPregnancyTraumaCancerPost-surgeryDiabetesHematomaThrombolytic therapyArterial thrombosisOlder ageGeneralized hospitalized patientThe rationale for the use of the
D-dimer as a negative predictor is that the formation of a thrombus requires both coagulation and fibrinolytic activation. D-dimer forms only with the activation of the coagulation system (fibrin formation) and the subsequent dissolution of the cross-linked fibrin clot.1,10 Breakdown products of the fibrin clot circulate in the blood and can be detected with monoclonal antibodies specific to D-dimer fragments. The presence of D-dimers suggests that a coagulation-fibrinolytic process is taking place, but does not necessarily confirm that a thrombus has formed.10Clinical assays for
D-dimerSince D-dimers form during a thrombotic process and in numerous other conditions, the D-dimer assay can be used to eliminate the presence of VTE. The assay must be sensitive and specific in the range for differentiation between the presence and absence of a thrombus. Therefore, the cutoff value must be established to exclude all patients with VTE, but not necessarily to include all patients without a thrombus.The D-dimer assay has been established utilizing three different methodologies. All three rely on monoclonal antibodies.5-7,9 The original assay was semiquantitative, utilizing visual macroscopic latex agglutination (used for diagnosis of DIC).10 The most sensitive quantitative D-dimer assays were based on the ELISA format, but are too time-consuming and require specialized equipment and training. The most practical method is based on the concept of microscopic latex agglutination. These assays based on light scattering are usually performed on coagulation instruments, eliminating special equipment needs, but still retaining the needed sensitivity.6-8Unfortunately, all three methods, and even any given method, may produce different results.3-8 These inherent problems occur due to differing monoclonal antibodies, lack of standard calibrators or standards, and inconsistent reporting units. As an example, the designations for reporting units are different and they have different values: 1 Fibrinogen Equivalence Unit (FEU) is approximately equal to 2 D-dimer units.The assay methodology is critical for its practical use in the clinical laboratory or in an outpatient-emergency department setting. Values spanning the cutoff must be accurate and sensitive. The assay must be inexpensive, available 24 hours a day, have a rapid turnaround time, and be performed on routine equipment. If it will be used in a setting other than a clinical laboratory, it must be able to be performed by nonlaboratory personnel.Several preanalytical and analytical variables, as with any coagulation test, may affect the D-dimer assay. Preanalytical variables, such as collection and storage conditions, are the same as for the other routine coagulation tests (PT and aPTT). Analytical variables affecting the quantitative D-dimer again are similar to the routine coagulation and chemistry tests, such as color and turbidity interference. These methodological artifacts must be recognized and corrected.Developing laboratory guidelines
for D-dimer assaysThe most practical commercial D-dimer assays to exclude VTE are based on microscopic latex agglutination using monoclonal antibodies. These antibodies have slightly different affinities and epitopes. Kits are developed specifically for a specific instrument. Therefore, the choice of test method is usually not based on the monoclonal antibody, but on the instrument available to the laboratory; i.e., the choice is based on instrumentation rather than sensitivity and specificity. Most methods have the capability of good negative-predictive value. If a choice of method and instrumentation is an option, then a review of the numerous comparison studies in the current literature should be made. This article does not deal with specific kits, but refers the reader to the literature.Most of the available assays can be automated and are relatively easy to set up and validate. The difficult aspect of establishing the D-dimer assay for exclusion of VTE is establishing the cutoff value. Each laboratory must establish its own cutoff value and cannot rely on a manufacturers recommended value or another laboratorys value. In addition, if the method is set up in the main laboratory and at an off-site location, then the cutoff value must be established for each instrument. The main criterion for establishing the cutoff value is that it must have 100 percent negative-predictive value
(Figure 4). Usually this value is low, near the average of the normal reference range. (The procedure for establishing the cutoff value is outlined in Table
2.) The important concept that cannot be overemphasized is establishing a 100 percent negative prediction that will exclude all individuals with thrombosis. After the initial conservative cutoff has been established, then re-evaluation periodically must be performed by a lookback comparison between D-dimer levels imaging data.
Table 2:
Outline of the procedure to establish the cutoff for 100 percent predictive value
- Establish D-dimer assay on instrumentation.
- Determine the reproducibility, intra- and inter-assay variability.
- Validate the assay as any other clinical assay.
- Establish the normal reference range for the D-dimer assay.
- Use normal subjects within the age range of the patients to be tested.
- All normal subjects should be healthy and not on anticoagulants.
- Must have at least 30 individuals.
- Determine the average and 2 SD.
- Determine D-dimer levels on at least 20 suspected VTE patients.
- Should be consecutive patients.
- Both positive and negative for VTE based on imaging studies.
- No anticoagulants.
- Plot data in ROC graph to establish initial cutoff value.
- Based on ROC cutoff, slightly decrease the cutoff value further. This is to make sure that all positive individuals are included in the image-tested group.
- Re-evaluate and adjust cutoff after evaluation of more patients (see steps 3 and 4 above).
- Re-establish after 30 patients.
- Re-evaluate after 50 patients.
- Re-evaluate after 100 patients.
- Re-evaluate every year and after changing methodology.
- Readjust cutoff every year with 50 patients.
- Start over.
of the D-dimerOnce the D-dimer assay has been validated with an established cutoff level, the assay can be used as a negative predictor for VTE. Guidelines for the use of the D-dimer should be developed with input from clinical staff to develop criteria for its use as a negative predictor.1,2,7 (The guidelines outlined in Table 3 will bring about significant cost savings.) During evaluation of the patient, the clinician categorizes the VTE risk into low, moderate, or high probability. Based on this clinical classification, subsequent testing is ordered. If the patient is classified as low or moderate probability, then a stat. D-dimer test is ordered. If the D-dimer level is above the cutoff value, then imaging procedures are performed. If those are positive, the patient is treated. However, if the D-dimer is below the cutoff value, then VTE is ruled out and other causes are investigated. The patient is not sent to imaging studies nor treated with anticoagulants. Patients with a high probability for VTE should be analyzed by imaging studies and
D-dimer testing bypassed. If positive for VTE, then appropriate anticoagulation therapy is given. If the imaging testing is negative, then other causes are investigated. In all negative cases in which the problem is not identified and persists for five to seven days, or becomes worse, then imaging analysis should be repeated.Table 3:
Clinical models for evaluation of suspected VTELow probability of
VTE:Clinically determined to be low probability by healthcare provider.Stat.
D-dimer assay.If D-dimer is positive (above cutoff),
then perform imaging studies.If imaging studies are positive, treat with anticoagulation.If imaging studies are negative, patient is evaluated for other causes.If D-dimer is negative (below cutoff),
no VTE. No imaging studies are performed.Patient is evaluated for other causes.If symptoms are not identified and persist, re-evaluate in 5 to 7 days.Moderate probability of
VTE:Clinically determined to be moderate probability by healthcare provider.Stat. D-dimer assay.If D-dimer is positive (above cutoff),
then perform imaging studies.If imaging studies are positive, treat with anticoagulation.If imaging studies are negative, patient is evaluated for other causes.If D-dimer is negative (below cutoff),
no VTE. No imaging studies are performed.Patient is evaluated for other causes.If symptoms are not identified and persist, re-evaluate in 5 to 7 days.High probability of
VTE:Clinically determined to be high probability by healthcare provider.Immediate imaging studies and no stat. D-dimer assay.If imaging studies are positive, treat with anticoagulation.If imaging studies are negativeNo VTE.Patient is evaluated for other causes.If symptoms are not identified and persist, re-evaluate in 5 to 7 days.Two major caveats must be incorporated into the procedure for the D-dimer assay: The D-dimer should be used with caution in hospitalized patients, since numerous disease processes and invasive procedures can elevate D-dimer levels without the presence of VTE. In these patients, reliance on clinical evaluation and imaging studies is more valuable.5,6,9 The D-dimer assay should not be used in patients on anticoagulant therapy (heparin or warfarin). Studies have demonstrated that anticoagulants
decrease circulating D-dimers and could possibility generate a false value below the cutoff, and VTE would be missed. It is not recommended that anticoagulated patients be tested for
D-dimer. Most hospitals which utilize the
D-dimer assay for VTE also use the D-dimer assay for confirmation of DIC. Since the range of detection necessary for the two assays is significantly different, we recommend that the hospital provide two assays and offer them as different tests for clinician ordering. In our hospital, we have both tests available; however, they are ordered as different tests with different values and ranges. We differentiate the two assays in the following way: Test name for ruling out VTE is D-dimer (Thrombosis), and the test name for DIC is D-dimer
(DIC).SummaryPatients with venous thrombosis (DVT or PE) have elevated D-dimer, a breakdown product of cross-linked fibrin. The determination of D-dimer levels is both a diagnostic and a cost savings tool to rule out VTE. The assay can be used to eliminate those individuals without VTE, but with low or moderate clinical suspicion. The D-dimer assay is inexpensive, automated, has a rapid turnaround time, and uses standard blue-top tubes. After appropriate validation, the assay can be 100 percent sensitive in ruling out DVT or PE, but it will not confirm the presence of VTE as numerous other diseases and procedures can increase levels. The assay should not be used routinely on inpatients or surgery patients. Caution should be used when interpreting results from patients on anticoagulation therapy, since lower D-dimer levels may be found. If properly used, the
D-dimer assay can save a healthcare facility significant money by eliminating imaging studies on patients with low or moderate suspicion of DVT or PE. Richard A. Marlar is director of the Routine and Special Coagulation Laboratories, Pathology and Laboratory Medicine, at the Denver Veterans Administration Medical Center, and associate professor in the department of pathology, University of Colorado Health Sciences Center, Denver.AcknowledgementsThe author would like to thank Susan Priem and the other personnel of the Denver VA Medical Centers Special Coagulation Laboratory for helping with these studies. This work was supported in part by a A Merit Review Grant and in part by Pathology Service of the Denver VA Medical Center.References1. Anderson DR, Wells PS. D-dimer for the diagnosis of venous thromboembolism. Curr Op Hematol. 2000;7:296-301.2. Janes S, Ashford N. Use of a simplified clinical scoring system and D-dimer testing can reduce the requirements for radiology in the exclusion of deep vein thrombosis by over 20%. Br J Haematol. 2001;112:1079-1082.3. Adams FG. The role of spiral computed tomography and D-dimer in pulmonary embolism. Scott Med J. 2001;46:7-8.4. Righini M, de Moerloose P, Reber G, et al. Should the D-dimer cut off value be increased in elderly patients suspected of pulmonary embolism? Thromb
Haemost. 2001;85:744.5. Anderson DR, Wells PS, Stiell I, et al. Management of patients with suspected deep vein thrombosis in the emergency department: combining use of a clinical diagnosis model with D-dimer testing.
J Emerg Med. 2000;19:225-230.6. Gosselin RC, Owings JT, Utter GH, et al. A new method for measuring D-dimer using immunoturbidity: a study of 255 patients with suspected PE and DVT. Blood Coag
Fibrinolys. 2000;11:715-721.7. Shitrit D, Heyd J, Raveh D, Rudensky B. Diagnostic value of the D-dimer test in deep vein thrombosis: improved results by a new assay and by using discriminate levels. Thromb Res. 2001;102:125-131.8. van der Graaf F, van den Borne H, van der Kolk, et al. Exclusion of deep vein thrombosis with D-dimer testing. Thromb
Haemost. 2000;83:191-198.9. Funfsinn N, Caliezi C, Dermarmels F, et al. Rapid
D-dimer testing and pre-test clinical probability in the exclusion of deep vein thrombosis in symptomatic outpatients. Blood Coag
Fibrinolys. 2001;12:165-170.10. Carey MJ, Rodgers GM. Disseminated intravascular coagulation: clinical and laboratory aspects. Am J Hematol. 1998;59:65-73.©
2002 Nelson Publishing, Inc. All rights reserved.