Transforming diagnostics in GI infections: The role of molecular testing
To take the test online go HERE. For more information, visit the Continuing Education tab.
LEARNING OBJECTIVES
Upon completion of this article, the reader will be able to:
1. Discuss GI disease healthcare statistics and testing strategies.
2. Describe the benefits of molecular testing in the diagnosis and management of GI diseases.
3. Describe molecular panel sizes and the benefits and limitations of each.
4. Discuss diagnostic strategies and the reimbursement challenges that contribute to limitations.
Diarrheal disease is a significant cause of morbidity and mortality, with the World Health Organization ranking it as the third leading cause of death in children under five years old globally.1 While acute gastroenteritis is infrequently fatal in the United States, it still poses a significant challenge to healthcare systems as a common and costly cause for healthcare visits.
One of the key difficulties in managing acute gastroenteritis is that the recommended treatment is usually supportive care despite significant symptoms affecting quality of life. This can often lead to pressure from patients who expect more from diagnostics since COVID-19 and who desperately want reassurances that everything is being done to identify the cause of their disease in hopes of a quick return to normalcy.
When testing is indicated, clinicians and laboratory professionals face mounting pressure to optimize diagnostic and therapeutic approaches to limit costs and antibiotic overuse. Molecular testing paired with diagnostic stewardship has revolutionized the management of gastrointestinal (GI) infections. This article explores how these cutting-edge strategies can enhance patient care, improve laboratory efficiency, and aid in the battle against antimicrobial resistance (AMR).
Advancements in molecular diagnostics testing
In recent years, extensive research has been conducted to evaluate diagnostic testing for infectious diarrhea, with molecular panels emerging as a powerful alternative to traditional stool cultures. These innovative panels offer superior diagnostic yield and dramatically reduce turnaround times, often delivering results within hours rather than the multi-day turnaround time frequently required with conventional stool cultures.
Studies have consistently demonstrated the improved yield of molecular syndromic panels, with one study finding a 35.5% positivity rate over the 6% yield observed with traditional methods.2 Multiplex polymerase chain reaction (PCR) panels, in particular, have shown enhanced detection rates across various pathogen types: bacteria (7.8% versus 2.9%), viruses (11.4% versus 0.63%), and parasites (2.4% versus 0.15%) when compared to standard techniques.3
Faster and more precise identification of pathogens contributes to antimicrobial stewardship efforts by allowing for the use of better-targeted therapies and the reduction of unnecessary antibiotic use. Rapid detection can also inform the implementation of infection control measures, thus preventing further spread, improving patient satisfaction by decreasing unnecessary isolation, and allowing for earlier detection of potential outbreaks. The comprehensive nature of these panels also helps to facilitate improved epidemiologic tracking of local trends allowing for better resource deployment.
The 2017 clinical practice guidelines for infectious diarrhea, published by the Infectious Diseases Society of America (IDSA) and the American College of Gastroenterology (ACG), recommend targeted testing in patients presenting with moderate-to-severe diarrhea persisting beyond seven days to clarify the etiology of illness. This approach optimizes diagnostic yield and clinical utility when testing is performed after a prolonged period of active symptoms while ensuring more judicious use of resources.4
While current guidelines acknowledge the value of molecular panels, they also highlight the scenarios where conventional culture methods are still necessary. They mention this in the context of recent trends in practice reflecting the growing demand for fast, accurate diagnostics that can facilitate timely treatment initiation and improve patient outcomes.
Panel sizes and special populations
Molecular panels for gastrointestinal pathogens are typically stratified into three categories based on the number of targets they contain. The size of these panels (i.e., number of targets) may directly impact reimbursement by payors. Small panels, which focus on detecting the most clinically significant pathogens, comprise five targets or fewer, and are generally reimbursed. However, this approach can often lead to the need for additional visits and tests if the initial test is negative.
Medium-sized panels, targeting 6 to 11 pathogens, have variable reimbursement rates and clinical adoption. While they may not be comprehensive enough for many special populations, they are generally considered suitable for the average patient with fewer limitations than small panels.
Large panels, encompassing 12 or more targets, have been facing an erosion in outpatient reimbursement with an increase in restrictions pushing these panels to inpatients and specific high-risk outpatient populations. These most commonly include immunocompromised individuals, pediatric and elderly populations, and those with recent travel history.
For example, in the inflammatory bowel disease (IBD) population, the value of large panels has been demonstrated in comparative studies. One such study evaluated the use of a large GI PCR panel compared to traditional work-up and found a statistically significant reduction in IBD therapy escalation (16% versus 29%; P < 0.01) and post-test endoscopic procedures (10% versus 18%; P = 0.04).6 (See Figure 1.) These findings suggest that the initial investment in advanced molecular diagnostics may lead to cost savings and improved patient outcomes in the long run for the IBD population.
Outside of special populations, the implementation of large PCR panels for inpatients has also resulted in significant benefits. For instance, in one study, a shorter duration of hospitalization was observed from the time of stool collection (3.4 days versus 3.9 days). This paired with a lower observed rate of additional stool testing orders and imaging studies underscores the potential to reduce unnecessary interventions and improve patient outcomes.
The incorporation of molecular panels in clinical practice represents a significant advancement in diagnosing gastrointestinal infections, offering superior detection rates across a spectrum of pathogens while also providing more information to support judicious antimicrobial use. Healthcare providers must navigate the balance between diagnostic comprehensiveness and economic considerations, particularly in light of reimbursement policies that may prioritize cost-effectiveness over clinical discretion. Ultimately, the integration of these advanced diagnostic tools requires an approach that ensures both improved patient care and practical constraints in healthcare delivery.
Navigating diagnostic strategies and reimbursement challenges
The diverse clinical presentations and pathogen types in GI infections necessitate a nuanced approach to diagnostic strategies. While PCR panels have gained prominence in many inpatient laboratory settings due to their high sensitivity and rapid turnaround time, they require supplementation with traditional diagnostic methods in some scenarios. Conventional techniques retain value when there is concern for novel pathogens or outbreak investigations. Moreover, while antibiotics are often not indicated, antimicrobial susceptibility testing should be available for instances where the results would affect patient care by determining the most appropriate therapeutic options.
The reimbursement landscape for GI pathogen panels has grown increasingly complex, with many payors implementing tighter criteria based primarily on panel size. These size categorizations are not rooted in evidence but are largely determined by payor policies. This disconnect underscores the need for ongoing dialogue between healthcare providers, payors, and policymakers to ensure reimbursement policies are aligned with best clinical practices and patient outcomes.
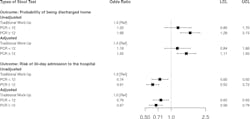
As mentioned, large PCR panels often represent a higher upfront cost at the index visit compared to smaller panels or conventional diagnostic approaches but have been associated with significant downstream benefits. in one large retrospective cohort study, these included reduced mean 30-day follow-up costs and a lower risk of hospitalization and associated antibiotic use.5 (See Figures 2 and 3) These findings suggest that despite higher upfront costs, implementation of molecular panels could lead to improved clinical outcomes, reduced healthcare overutilization, and enhanced antimicrobial stewardship.
Regional differences and future directions
The arbitrary categorization of molecular diagnostics by payors necessitates careful consideration of regional patterns in pathogen prevalence, which can significantly impact the optimal design and composition of diagnostic panels. Consequently, there is a growing need for more adaptable testing platforms that can accommodate local epidemiologic trends.
In response to recent shifts in reimbursement trends, several diagnostic companies are actively developing mid-sized panels. This emerging market segment aims to bridge the gap between more limited small panels and comprehensive large panels, attempting to strike a balance between diagnostic breadth and cost-effectiveness for low-risk populations in the outpatient setting. As processes for GI pathogen detection continue to evolve, it is crucial to consider the diverse needs of both general and specialized patient populations in selecting diagnostic panels and designing testing algorithms with the flexibility to serve your patient population.
Implementing advanced molecular testing methodologies has emerged as a critical consideration in managing GI infections and the ongoing battle against AMR. Recent literature provides compelling evidence supporting the superiority of molecular panels over conventional techniques for most patient populations. As the field of GI diagnostics continues to advance, the integration of these innovative tools promises to enhance patient care and infection control practices, improve laboratory efficiency, and contribute to global efforts in combating AMR.
References
1. Diarrhoeal disease. Who.int. Accessed September 26, 2024. https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease.
2. Cybulski RJ Jr, Bateman AC, Bourassa L, et al. Clinical impact of a multiplex gastrointestinal polymerase chain reaction panel in patients with acute gastroenteritis. Clin Infect Dis. 2018;13;67(11):1688-1696. doi:10.1093/cid/ciy357.
3. Axelrad JE, Freedberg DE, Whittier S, Greendyke W, Lebwohl B, Green DA. Impact of gastrointestinal panel implementation on health care utilization and outcomes. J Clin Microbiol. 2019;57(3). doi:10.1128/JCM.01775-18.
4. Riddle MS, DuPont HL, Connor BA. ACG Clinical Guideline: Diagnosis, treatment, and prevention of acute diarrheal infections in adults. Am J Gastroenterol. 2016;111(5):602-622. doi:10.1038/ajg.2016.126.
5. Moon RC, Bleak TC, Rosenthal NA, et al. Relationship between diagnostic method and pathogen detection, healthcare resource use, and cost in U.S. adult outpatients treated for acute infectious gastroenteritis. J Clin Microbiol. 2023;61(2):e0162822. doi:10.1128/jcm.01628-22.
6. Hong S, Zaki TA, Main M, et al. Comparative evaluation of conventional stool testing and multiplex molecular panel in outpatients with relapse of inflammatory bowel disease. Inflamm Bowel Dis. 2021;27(10):1634-1640. doi:10.1093/ibd/izaa336.
7. Beal SG, Tremblay EE, Toffel S, Velez L, Rand KH. A gastrointestinal PCR panel improves clinical management and lowers health care costs. J Clin Microbiol. 2018;56(1). doi:10.1128/JCM.01457-1.
To take the test online go HERE. For more information, visit the Continuing Education tab.
About the Author

David Allen, PharmD, BCIDP
is a Field Medical Director at bioMérieux. In this role, he works with key opinion leaders (KOLs) from large Integrated Delivery Networks and National Accounts on bridging the gap between the patient care needs of these KOLs and the pipeline development process. He is a graduate of Virginia Commonwealth University School of Pharmacy and previously practiced as an Infectious Diseases Clinical Pharmacy Specialist, with the majority of his time as the lead pharmacist for the antimicrobial stewardship program at the Inova Health System.