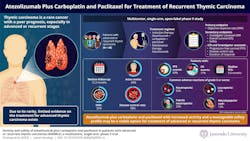
Researchers from Japan have evaluated the efficacy and safety of atezolizumab plus carboplatin and paclitaxel in patients with advanced or recurrent thymic carcinoma. The findings revealed that this combination exhibited a manageable safety profile and may redefine treatment strategies, offering new hope for patients with recurrent thymic cancer.
A team of researchers led by Associate Professor Takehito Shukuya from the Department of Respiratory Medicine, Juntendo University, Japan along with Dr. Tetsuhiko Asao, Dr. Tomoyasu Mimori, and Prof. Kazuhisa Takahashi from Juntendo University, Japan, conducted the MARBLE study to evaluate the combination of atezolizumab, an immune checkpoint inhibitor, with carboplatin and paclitaxel in patients with advanced or recurrent thymic carcinoma. The findings of the study were published in Volume 26, Issue 3 of The Lancet Oncology.
This multicenter, single-arm, phase II clinical trial was conducted across 15 hospitals in Japan and enrolled 48 patients with histologically confirmed advanced or recurrent thymic carcinoma. During the induction phase, patients received a combination of atezolizumab, carboplatin, and paclitaxel every three weeks for up to six cycles. Those with non-progressive disease transitioned to a maintenance phase, receiving atezolizumab every three weeks for up to two years.
Dr. Shukuya explains, “The MARBLE study delivered promising results. With a median follow-up of 15.3 months, the combination therapy achieved an objective response rate of 56% and a median progression-free survival (PFS) of 9.6 months, outperforming historical chemotherapy outcomes. The disease control rate reached 98%, with 56% of patients achieving partial responses and 42% maintaining stable disease.”
The safety profile was consistent with the known effects of atezolizumab, carboplatin, and paclitaxel, with no new safety concerns or treatment-related deaths. Adverse events were manageable, with the most common severe events being neutropenia, leukopenia, maculopapular rash, and febrile neutropenia. Notably, patients with higher programmed cell death ligand 1 expression on tumor or immune cells exhibited longer PFS, highlighting its potential as a predictive biomarker for treatment response.