A national, multicenter clinical trial (BMT CTN 1507) of low-dose haploidentical (half-matched) bone marrow transplant to treat severe sickle cell disease found the treatment to be safe and curative for adults with serious sickle cell-related health complications.
The findings from the phase II clinical trial were featured Dec. 12 as a high-impact study (abstract #LBA4) at the annual meeting of the American Society of Hematology (ASH).
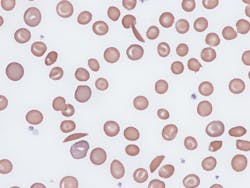
The clinical trial included 42 individuals with sickle cell disease. Most participants were African American (92.6%), and the median age was 22. Of the 42 participants, 95% were still alive two years after transplant, and 88% have not seen their sickle cell disease return and are considered cured.
Patients in the clinical trial — sponsored by the National, Heart, Lung, and Blood Institute and the National Cancer Institute — were treated with a reduced-intensity (low dose) haploidentical bone marrow transplant at 19 hospitals across the U.S. In this type of bone marrow transplant, the donated bone marrow comes from a half-matched donor, such as a patient’s parent, sibling or child. Other relatives, including a nephew, niece, aunt or uncle, are also often suitable donors. Patients were treated with low-dose therapy to prepare them for transplant, and were given post-transplant cyclophosphamide, a drug that earlier research has proven to stave off graft-versus-host disease, a complication in which the immune cells in the donor marrow attack their new host, the patient.
In the reduced intensity, haploidentical transplant study, serious side effects were uncommon. They included one graft failure; moderate to severe graft-versus-host disease (26.2%) and two deaths in the first year post-transplant.