Proteins suggest a path to reduce drug resistance in a form of cancer
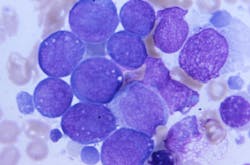
A new study draws on a field of science known as proteogenomics to try to improve the outlook of acute myeloid leukemia (AML). In a paper published January 16 in Cell Reports Medicine, scientists report new findings about how drug resistance in some AML patients develops and how doctors might someday stop or slow the process.
The research comes from a team of researchers from the Department of Energy’s Pacific Northwest National Laboratory and Oregon Health & Science University.
The PNNL-OHSU team is studying thousands of proteins that could play a role in AML. Proteins are the body’s molecular workhorses, ferrying nutrients and other supplies back and forth between cells, turning genes on or off, and maintaining dozens of basic body processes. Even though genes get the glory, they do little directly to keep our bodies going. That’s the job of proteins. For nearly 20 years, study author Karin Rodland of OHSU, formerly of PNNL, has been a pioneer exploring the role of proteins in health and disease, building a program with OHSU and PNNL colleagues to study AML.
In the latest study, a team led by Sara Gosline, a data scientist and computational biologist at PNNL, did an exhaustive study of the protein activity in 210 patients with AML. Altogether, the team measured levels of nearly half a million pieces of proteins from more than 9,000 proteins in patients’ blood samples. The team combined those findings with extensive data already known about the disease—the genes and mutations involved, the molecular messengers that indicate which genes are active, and the effects of 46 drugs on AML patients, along with information about how the disease progressed in those patients.
Gosline and colleagues, including first author James Pino of PNNL, deployed artificial intelligence, using several machine learning algorithms to make sense of the data.
While the study yielded a load of data about what happens in the body of an AML patient, one finding stood out, pointing to a possible way to sidestep or delay drug resistance for some patients.
The team showed that treatment with quizartinib, approved last year to treat AML, can shift how cancer cells respond to other drugs often used in combination to treat patients.
Specifically, the team found that when patients on quizartinib stop responding to venetoclax, doctors might consider switching to another drug, panobinostat. It’s an example of how proteogenomic information could alter the roadmap that doctors use to navigate which medications patients receive at different stages of the disease.
Ultimately, the team focused on 147 proteins and specific molecular locations known as phosphosites that play a key role in determining which proteins are turned on and which are off.
Using just the protein data, the team sorted the samples into four distinct groups that predicted how the patients fared. Patients whose samples placed them in one of the groups had a better prognosis than the others, surviving far more than five years. Doctors hope that this type of information will eventually become available in the clinic. That would allow some patients who do not need aggressive therapies with severe side effects to avoid them while assuring that patients who have the worst prognosis are treated as aggressively as possible.