Point-of-care testing (POCT) technology continues to advance at a fast pace, making it easier to shrink complex testing platforms into point-of-care (POC) devices. Though not without its challenges, testing at a molecular level far surpasses the accuracy of other POCT methodologies. Molecular POCT devices allow quick, easy-to-use testing in near-patient scenarios where a rapid diagnosis can be the difference between treating one patient and treating a multitude of patients who become infected because the initial diagnosis is delayed.
Molecular testing is a broad term that refers to the detection and/or quantification of specific DNA or RNA sequences in a specimen. Molecular tests are used to detect microorganisms, look for genetic mutations associated with certain diseases and cancers, perform paternity tests, and much more. Highly complex molecular testing is performed in molecular or microbiology specialty laboratories by trained laboratory professionals.
Basic principle of molecular testing
The starting principle behind molecular testing involves multiplying (or amplifying) the amount of DNA or RNA within a specimen by thousands to millions of times prior to analyzing. DNA is amplified using cycling methods, such as polymerase chain reaction (PCR) or isothermal amplification. This means that samples with only a few hundred infectious particles can be amplified billions of times, which increases the likelihood of detection and potentially compensating for suboptimal sample collection.
The amplification of DNA/nucleic acids is achieved using naturally occurring enzymes (proteins). DNA polymerase is one of the key enzymes used in this process, which is the basis for the PCR methodology. Other enzymes can be used for amplification, and these are typically grouped under the generic label of isothermal nucleic acid amplification tests (INAAT). The amplification step makes molecular testing methodologies more sensitive than immunological assays, as each cycle of amplification doubles the amount of DNA in the sample. PCR testing involves amplification achieved through temperature cycling, while isothermal amplification assays use a constant reaction temperature for the amplification that results in a shorter run time than PCR.
PCR versus isothermal
PCR assays use fluorescence to detect the amount of amplified DNA in real time. With each cycle of PCR, more dye molecules are released, so the fluorescence increases proportionally to the amount of target amplicon. In real-time PCR, the amount of target DNA present in the sample typically determines the number of PCR cycles necessary. This number is called the cycle threshold or Ct value.1 Subsequently, Ct levels are inversely proportional to the amount of target nucleic acid in a sample.
Meanwhile, there are a multitude of types of isothermal molecular technologies, including:
- Helicase-dependent amplification (HDA)
- Loop-mediated isothermal amplification (LAMP)
- Nicking enzyme amplification reaction (NEAR)
- Reverse transcription recombinase polymerase amplification (RT-RPA)
- Rolling circle amplification (RCA)
- Transcript-mediated amplification (TMA)
Although these methods vary, they have some commonalities. For example, because the nucleic acid strands are not amplified with heat, isothermal methods use an alternative method for primer binding and amplification reaction — a polymerase with strand-displacement activity. The polymerase is also used to separate the strand that is still annealed to the target gene sequence.
Isothermal nucleic acid amplification, used in many molecular diagnostic platforms (and in POCT), speeds the testing process by eliminating the need for thermal cycling. For example, LAMP uses strand-displacing DNA polymerase and primers to amplify specific DNA sequences.2 RT-RPA uses recombinase, single strand binding protein, DNA polymerase, and reverse transcriptase to amplify the RNA target. For each of these methodologies, the output is interpreted via fluorescent or colorimetric reporters and lateral flow strip platforms to achieve decipherable test results.
The high level of reliability and accuracy that molecular testing techniques offer typically comes with a longer turnaround time (TAT), which is attributed to batch testing, complex multistep testing, and predetermined testing schedules. PCR methodologies, considered the gold standard for RNA virus detection, can take up to four hours for results and require expensive thermal cyclers.2 In addition, traditional molecular diagnostic methodologies require sophisticated infrastructure, expensive reagents, stable electrical power, and highly skilled staff.
Traditional (non-molecular) POCT
Generally speaking, POCT allows for rapid diagnosis and subsequent timely treatment. Rapid, easy-to-administer POCT has long been used to detect infectious disease antigens or antibodies, such as influenza, mononucleosis, and group A streptococcus (GAS). However, despite offering a quick TAT, many of these assays come with a less than ideal sensitivity and specificity trade-off. Conventional, non-molecular POCT can have suboptimal limits of detection, resulting in false negatives for samples with low viral or bacterial load. Because of this lower sensitivity, these tests typically require a confirmatory test to rule out false negatives. This scenario sets the stage for the rapid TAT combined with higher sensitivity that molecular POCT methodologies offer.
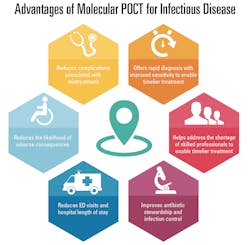
Molecular POCT is much faster than lab-based molecular tests and more accurate than existing non-molecular POCT. The precision and accuracy of molecular POCT gives clinics or other ambulatory care centers the ability to deliver a standard of care equivalent to a tertiary care center.3
Infectious disease testing
During the last three decades, more than 30 new infectious diseases have been identified, making it imperative to have a reliable method to identify the responsible pathogens.4 Access to sensitive and rapid infectious disease assays is essential for accurate diagnosis, effective treatment, and timely infection control. Although antigen-based POC tests offer a quick TAT, the testing has a relatively low sensitivity and specificity (compared to culture) and can be difficult to interpret, potentially leading to erroneous results. As such, the recommendation is to reflex negative results to a confirmatory molecular method.
Group A Streptococcus (GAS)
Annually, there are approximately 11 million pediatric care visits for pharyngitis, of which GAS — the type of pharyngitis that requires treatment — accounts for 15-30%.5 Traditional culture methods offer a TAT of 24 to 48 hours, causing a significant delay in definitive diagnosis. A rapid, accurate diagnosis for GAS pharyngitis is vital to decreasing transmission and avoiding more serious complications like acute rheumatic fever.
With rapid antigen POCT and its requisite confirmatory testing, an empiric therapy may be employed which can contribute to the unnecessary use of antibiotics. Due to this testing conundrum, unfortunately, antibiotics are prescribed for approximately 60% of all pharyngitis cases, in spite of only 15-30% of pharyngitis cases actually being caused by GAS.5 In contrast to traditional POCT, molecular POCT for GAS provides more reliable and accurate results that enable faster diagnosis, treatment and eliminate the delay and cost for confirmatory testing.
Influenza
Another respiratory illness that greatly benefits from rapid and highly accurate molecular POCT is Influenza. According to the estimates from the Centers for Disease Control and Prevention (CDC), there were approximately 490,600 hospitalizations and 34,200 deaths attributed to influenza during the 2018–2019 season. Specific to pediatrics, there were more than 46,000 hospitalizations and 136 deaths.6
To achieve best patient care, influenza requires a rapid, highly accurate diagnostic test, so an antiviral treatment can be administered within 48 hours of symptoms. Antigen-based POCT for influenza is frequently used in outpatient settings but is significantly less sensitive compared to molecular methods. The rapid TAT and accuracy of molecular influenza testing allows antivirals to be administered in a timely manner, subsequently preventing unnecessary hospitalizations and antibiotic prescriptions.3
Molecular POCT for COVID-19
Response to the COVID-19 pandemic has also been challenged by delays associated with centralized laboratory PCR testing. In hospitals, these delays lead to poor patient flow and nosocomial transmission. To fulfil the demand for rapid diagnoses during disease outbreaks, the healthcare industry needs POCT that is affordable, fast, and deployable in the field.2 The rapid, accurate test results that molecular POCT methodologies offer are extremely beneficial in a public health crisis, such as a pandemic. Molecular POCT is associated with faster results, improvements in infection control measures, and better patient flow, as compared with centralized laboratory PCR testing.7 For public health emergencies, molecular POCT can be used to achieve accurate, economical diagnoses, promoting early detection and mitigation to better control an infectious disease outbreak. A rapid, accurate, cost-effective device benefits individual patients and the public by reducing transportation needs, lowering the spread of infection, and reducing the cost of testing.
Laboratory staff shortages
Another factor driving the demand for molecular POCT is the scarcity of skilled laboratory professionals available to perform traditional molecular testing. Laboratory professionals have faced a workforce shortage for many years, with the competition to hire qualified technologists more challenging than ever. The Bureau of Labor Statistics estimates that an additional 35,100 jobs will be needed between 2018 and 2028, which does not include job openings due to retiring workers.8
The development and implementation of point of care molecular testing, many of which are CLIA-waived and subsequently easy to use, allows testing to take place near patients in clinics, EDs, pharmacies, etc. — testing that previously could only be accomplished with specialized staff.
Antibiotic stewardship
In addition, the use of more sensitive and specific molecular tests at the POC promotes more appropriate use of antibiotics and improves overall infection control. Antimicrobial resistance is an ongoing major public health issue. Our healthcare system is tasked with improving stewardship of antibiotics; meaning, swift administration of the appropriate antibiotic within an effective time frame and ensuring that antibiotics are not prescribed for illnesses that do not require them. However, effective antibiotic stewardship is complicated by the fact that initial antibiotic use is often empiric because the provider does not have definitive results that identify the pathogen for two to three days post empiric prescription.9 The consensus among experts is that antibiotic stewardship can be improved by implementing POCT diagnostics to rapidly identify bacterial pathogens.9 For example, POCT for pharyngitis has become widely available in pharmacies and is considered an effective part of the strategy to contain antibiotic resistance and contribute to antimicrobial stewardship.10 Successful implementation of rapid POCT has the potential to help prevent the spread of infectious diseases and impede antimicrobial resistance.11
Access to sensitive and rapid infectious disease assays is essential for accurate diagnosis, effective treatment, and timely infection control. Innovations in molecular POCT are allowing molecular testing to expand from specialty molecular diagnostics laboratories into clinical laboratories, clinics, and any testing location near the patient’s side. The rapid TAT of POCT combined with the superior sensitivity and specificity of molecular methodologies affords the best scenario for diagnosis and containment of contagious infectious diseases. For public health emergencies, molecular POCT can be used to achieve accurate, economical diagnoses, promoting early detection and mitigation to better control an infectious disease outbreak.
Reference List
- Dunn J, Brown C, Jung J. Laboratory diagnostics and testing guidance for COVID-19. Medscape. Published Jun 18, 2021. Accessed August 2, 2021. https://emedicine.medscape.com/article/2500138-overview#a3.
- Subsoontorn P, Lohitnavy M, Kongkaew C. The diagnostic accuracy of isothermal nucleic acid point-of-care tests for human coronaviruses: A systematic review and meta-analysis. Sci Rep 10, 22349 (2020). https://doi.org/10.1038/s41598-020-79237-7.
- Larkin P, Garner O. Molecular point-of-care testing in clinical laboratories. CLN. July 2020. Accessed August 2, 2021. www.aacc.org/cln/articles/2020/july/molecular-point-of-care-testing-in-clinical-laboratories.
- Hansen S, Wahed A. Point-of-care or point-of-need diagnostic tests: time to change outbreak investigation and pathogen detection. Trop Med Infect Dis. 2020 Sep 25;5(4):151. doi: 10.3390/tropicalmed5040151.
- Thompson T, McMullen A. Group A Streptococcus testing in pediatrics: the move to point-of-care molecular jesting. J Clin Microbiol. 2020 May 26;58(6):e01494-19. doi: 10.1128/JCM.01494-19.
- Estimated influenza illnesses, medical visits, hospitalizations, and deaths in the United States — 2018–2019 influenza season Influenza (Flu). Centers for Disease Control and Prevention. Accessed August 2, 2021. www.cdc.gov/flu/about/burden/2018-2019.html
- Brendish N, et. al. Clinical impact of molecular point-of-care testing for suspected COVID-19 in hospital (COV-19POC): A prospective, interventional, non-randomised, controlled study. Lancet Respir Med. 2020 Dec;8(12):1192-1200. doi: 10.1016/S2213-2600(20)30454-9.
- U.S. Bureau of Labor Statistics. Occupational Outlook Handbook. Clinical Laboratory Technologists and Technicians. 2021. Accessed August 2, 2021. www.bls.gov/ooh/healthcare/clinical-laboratory-technologists-and-technicians.htm#tab-1
- Dhesi Z, et. al. Rapid and point-of-care testing in respiratory tract infections: an antibiotic guardian? ACS Pharmacol Transl Sci. 2020 Jun 12; 3(3): 401–417. doi: 10.1021/acsptsci.0c00027.
- Essack S, et. al. Point-of-care testing for pharyngitis in the pharmacy. antibiotics (Basel). 2020 Oct 28;9(11):743. doi: 10.3390/antibiotics9110743.
- Hays, J.P., Mitsakakis, K., Luz, S. et al. The successful uptake and sustainability of rapid infectious disease and antimicrobial resistance point-of-care testing requires a complex ‘mix-and-match’ implementation package. Eur J Clin Microbiol Infect Dis. Eur J Clin Microbiol Infect Dis. 2019 Jun;38(6):1015-1022. doi: 10.1007/s10096-019-03492-4.