Urinary Tract Infection (UTI) is among the leading causes for treatment in adult primary care medicine and represents a significant proportion of antibiotic prescriptions. A UTI can involve any part of the urinary system, including the lower urinary tract – urethra (urethritis) and bladder (cystitis) – and the upper urinary tract – ureters (ureteritis) and kidneys (pyelonephritis). UTI impacts both genders, however, women are much more vulnerable due to their anatomy and reproductive physiology. Escherichia coli accounts for about 80-85 percent of all UTIs, followed by Staphylococcus species, accounting for 10-15 percent. Other bacterial pathogens – including Klebsiella, Pseudomonas, Proteus, and Enterococcus species – are also infrequently implicated. More rarely, infections may be from fungal or viral pathogens that would require alternative treatment strategies.1
Further sub-classifications of UTIs are based on location of the infection, presence or absence of symptoms, and the presence of relevant complicating factors that dramatically increase the patient risk profile. Complications can include all UTIs in children, men and pregnant women, renal insufficiency or transplant, diabetes mellitus, physical obstruction, immune compromised patients, etc.2
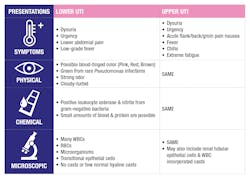
Symptoms
Symptoms of lower UTIs include burning or pain while urinating (dysuria), frequent urge to urinate with little or no volume (urgency), lower abdominal cramping or pain, and possible low-grade fever. Symptoms of upper UTIs are more severe and can include acute flank, back or groin pain, dysuria, urgency, fever, chills, nausea, and extreme fatigue. 1
Physical Presentation
Examination of the physical presentation of urine is an ancient practice that continues to provide valuable information in a modern clinical diagnostic setting.
Color
Normal urine color ranges from pale yellow to amber due to the pigment urochrome, a metabolic byproduct of heme. The color of UTI affected urine can have a blood-tinged color of red, pink or brown due to the presence of RBCs and/or hemoglobin caused by inflammation and irritation from an active infection. A Pseudomonas aeruginosa infection can uniquely result in green urine through the production of pyocyanin.1
Odor
Normal urine will have a faint smell that is not particularly harsh. UTI affected urine can have a pungent smell caused by the bacterial metabolism of urea into ammonia at the site of infection in the urinary tract. The smell can also be foul from the accumulation of pus, protein decay, and bacteria. It is important to note if the urine is fresh because improperly stored, unpreserved urine samples can develop a similar odor from contamination.
Clarity
Freshly voided urine is normally clear. UTI affected urine can be visibly cloudy due to an increase of suspended particles that scatter light. The makeup of the particles should be characterized by microscopy to determine if the constituents are pathologic.
Chemical Presentation
The chemical examination of urine most commonly employs the use of urinalysis dipsticks that contain discrete reagent pads that quickly detect the presence of specific analytes in the urine sample. Urinalysis dipsticks provide rapid, semi-quantitative diagnostic results that can be performed in most clinical settings.
UTI affected urine may react positively for leukocyte esterase activity due the inflammatory response elicited by the active infection. The leukocyte reagent pad reacts to the presence of leukocyte esterase enzymatic activity that can cleave an ester to form an aromatic compound that cascades through a diazo coupling reaction to yield a violet dye compound. The resulting color change in the reagent pad can be read visually, or with a dedicated reader, with the intensity being proportional to the concentration of leukocyte esterase in the original sample.
The presence of nitrite in urine is a strong indication of gram-negative bacterial UTI. Nitrates (NO3-) are consumed in the diet and are excreted in the urine without being converted to nitrite (NO2-). Nitrate-reducing bacteria, including E. coli, can switch from using oxygen to nitrate for respiration, releasing nitrite in the process. The reagent pad contains an aromatic amine compound that reacts with nitrite to produce a diazomium salt which cascades through a similar diazo coupling reaction to yield a pink dye compound. Unlike the leukocyte reaction, the nitrite assay is qualitative where any degree of pink color is considered a positive and does not correlate to the severity of the UTI. It is important to note that not all organisms that can cause UTI are able to convert nitrate into nitrite. A negative result, therefore, does not rule out UTI from a non-nitrate reducing bacteria (such as Enterococcus), fungi or virus.
Lastly, urine dipsticks may also detect the presence of small amounts of blood and protein in UTI-affected samples, resulting from inflammation and irritation to the urinary tract. While these findings are not specific to UTI, they are useful for ongoing assessments of UTI progression and resolution.
Screening tests for leukocytes or nitrite are not replacements for gold standard bacteriological urine cultures, which can identify and quantify the pathogen, ultimately providing information for the best treatment plan. The Leukocyte-Nitrite test combination is a very useful rapid tool that has been shown to have a sensitivity of 79.2 percent and a specificity of 81 percent for urine specimens with a bacterial count of >105 CFU/mL. Negative results from the combination have an excellent negative predictive value of 94.5 percent.3 The low-cost urinalysis dipstick allows for broad surveillance that can help identify patients with asymptomatic bacteriuria that may progress into a more severe condition. It also allows for a simple method to monitor the effectiveness of treatment.
Microscopic Presentation
The microscopic evaluation of urine is useful to confirm suspected UTI cases after physical and chemical analysis described above. These results provide added information to help confirm a diagnosis. It is important to understand if any physical or chemical findings originate in the urinary tract or are the result of external contamination. Microscopic analysis is particularly useful to begin to distinguish between lower and more serious upper UTI that may lead to a life-threatening acute pyelonephritis condition.
The detection of many WBCs in urine (leukocyturia) is a diagnostic hallmark of UTI and is the factor that contributes to observations of cloudy urine and a positive leukocyte esterase test. It is important to note that both bacterial and non-bacterial causes of inflammation can result in leukocyturia. Neutrophils are the most commonly found WBC type in UTI affected urine and are characterized as 10-20 µm spherical cells with cytoplasmic granules and segmented nuclei.1 Other WBC types, such as eosinophils, will predominate in cases of acute interstitial nephritis and lymphocytes in cases such as kidney transplant rejection.4
The observation of microorganisms in urine sediment is an additional hallmark of UTI, and one that is is useful to determine the causative pathogen. Bacteria found in urine can be rod-shaped (bacilli) or rounded (cocci). As urine is normally sterile, the presence of bacteria indicates either a UTI or contaminated sample. In cases where numerous bacteria are detected, in the absence of leukocytes or leukocyte esterase, the sample was likely contaminated or mishandled. Microscopic evaluation can also detect other UTI pathogens such as yeast, Trichomonads, and parasites such as Giardia and Pinworm.
RBCs are also commonly found in UTI affected samples which contribute to the changes in urine color and positive blood test described above. There are many unrelated conditions that can contribute to an increase of RBCs in urine (hematuria). In general, any source of inflammation or irritation of the urinary tract can result in hematuria. It is important to rule out potential sources of contaminate blood from vaginal secretion or hemorrhoids that can cause false hematuria positives.1
Other microscopic observations of urine sediment are particularly useful to differentiate between lower and upper UTI. The more common lower UTI can present with transitional epithelial cells that line the bladder and urethra. These can be sloughed off into the urine due to the inflammation caused by an offending UTI. In contrast, upper UTI can present with renal tubular epithelial cells (RTE) that line the proximal and distal convoluted tubules and collecting ducts. The presence of RTE in urine is the most clinically significant epithelial cell that can be found in urine and provides a strong indication of renal damage.5
The presence of urinary casts is another distinguishing characteristic that can differentiate between lower and upper UTI. Casts are cylindrical secretions composed of Tamm-Horsfall immunoprotein that form in the lumen of the distal tubes and collecting ducts of the nephron. Small numbers of clear hyaline casts or granular casts can be found in normal urine. Urine samples affected by a lower UTI will typically present with no casts, or with a few normal casts. A diagnostic hallmark of upper UTI acute pyelonephritis is the presence of WBC incorporated casts.5
Summary
As infections of the urinary tract are one of the most frequent reasons for treatment in primary medical care, it is critical to understand the various diagnostic hallmarks of UTI that allow for rapid assessment and treatment. Diagnosis solely based on clinical symptoms is often wrong, and diagnostic precision is dramatically increased using physical examination of the urine, chemical detection of leukocyte esterase and nitrite using urinalysis dipsticks, and microscopic sediment analysis.6 Quality control products allow for the verification of laboratory equipment, reagents, and operator technique associated with the diagnosis of UTI. This QC material is designed to elicit clinically significant negative and positive for all the typical urinalysis dipstick analytes, including leukocyte esterase and nitrite. It also contains intact WBCs, RBCs, calcium oxalate crystals and E. coli bacteria that are ideal for verifying the centrifugation, concentration, and slide preparation necessary for microscopic analysis, or ensure the performance of automated microscopy analyzers. The use of QC is a critical measure to ultimately provide critical information in a timely manner so that appropriate actions may be taken to improve patient outcomes. Resources such as the free “Urinalysis Made Simple” mobile application is an excellent tool for laboratory professionals, teachers, and students to understand the various physical, chemical, and microscopic presentation of urine for a variety of conditions.
References
- Brunzel N, Fundamentals of Urine & Body Fluid Analysis. 3rd Ed. St. Louis: Saunders; 2012.
- Medina M, Castillo-Pino E. An introduction to the epidemiology and burden of urinary tract infections. Ther Adv Urol. 2019 May 2. doi:10.1177/1756287219832172
- Pfaller MA, Koontz FP. Laboratory evaluation of leukocyte esterase and nitrite tests for the detection of bacteriuria. J Clin Microbiol. 1985;21(5):840-842. doi:10.1128/JCM.21.5.840-842.1985.
- R. Willi Grunewald, G. Martin Fiedler, Birgit Stock, Julia M. Grunewald, Gerhard A. Müller, Immunocytological determination of lymphocytes and monocytes/macrophages in urinary sediments of renal allograft recipients, Nephrology Dialysis Transplantation. 2000; 15 (6): 888–892. https://doi.org/10.1093/ndt/15.6.888
- Haber M, Novak R, Glassy EF. Color Atlas of the Urinary Sediment: An Illustrated Field Guide Based on Proficiency Testing. College of American Pathologists; 2010.
- Schmiemann G, Kniehl E, Gebhardt K, Matejczyk MM, Hummers-Pradier E. The diagnosis of urinary tract infection: a systematic review. Dtsch Arztebl Int. 2010;107(21):361-7. doi: 10.3238/arztebl.2010.0361.
About the Author

Brian Fernandez
serves as Director of Research and Development for Redondo Beach, California-based Quantimetrix.