Understanding hemostasis and hemostasis testing
As soon as a blood vessel is ruptured following an injury, a series of physiological events, called hemostasis is triggered. Hemostasis is a complex, dynamic mechanism that stops bleeding from damaged or injured blood vessels by balancing procoagulant and anticoagulant forces.1, 2 Parts of the body involved in hemostasis are the circulatory/vascular system that contains the blood vessels; the liver that produces clotting factors; and bone marrow that produces platelets.
Hemostasis is important for the following reasons:
- Prevents excessive and uncontrolled blood loss
- Helps to maintain homeostasis
- Prevents accumulation of blood in internal organs during the bursting of blood vessels internally by quickly checking the bleeding process
- Triggers the healing process of the ruptured vessels
- Coagulation system works in tandem with the immune system to maintain health and are also involved in various pathological conditions3
The process of hemostasis
The entire process can be broadly divided into the following stages:
Primary hemostasis involves two main physiological events — vasoconstriction and platelet plug formation.
With the rupture of the blood vessel, endothelin-1 (a vasoconstrictor) is released from the damaged endothelium of the blood vessel that causes vasoconstriction. Other chemical components like sub-endothelial collagen, ATP (adenosine triphosphate), von Willebrand factor (vWF), and inflammatory mediators also get released into the circulatory system, which also promote vasoconstriction
The sub-endothelial collagens and von Willebrand factors facilitate platelet accumulation and adhesion in the ruptured site. The attached platelets rupture and release serotonin, ADP (adenosine diphosphate), and thromboxane A2. All these components of the platelets also enhance vasoconstriction. During the rupture of the blood vessel, local pain receptors initiate reflexes that further promote the vascular spasm.
The platelets bound with collagen and endothelial lining form a temporary seal called the platelet plug. The platelet plug seals the vessels temporarily and prevents or slows down the rate of blood flow. The platelet plug activates the clotting factors and initiates clotting — the secondary hemostasis.
Secondary hemostasis involves sequential activation of procoagulant proteins or coagulation cascade.4
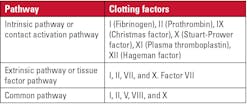
Secondary hemostasis follows two main coagulation pathways, intrinsic and extrinsic, that subsequently converge to form a common pathway that activates the conversion of fibrinogen to fibrin.
The process of secondary hemostasis or coagulation takes place through a series of clotting factors as listed below:
The process of secondary hemostasis takes place in the following order:
1) Activation of clotting factors, 2) conversion of prothrombin into thrombin, and 3) conversion of fibrinogen into fibrin fiber.
Tertiary hemostasis or fibrinolysis5 — Subsequent to the formation of a blood clot, healing of the ruptured vessels begins. Once the blood vessel is completely healed, the fibrin is lysed in a complex process called fibrinolysis. Broadly speaking, fibrinolysis occurs in two steps:
- Generation of plasmin by plasminogen activators: Factor XII, protein catabolizing enzymes, and other co-factors activate the plasminogen into plasmin
- Digestion of fibrin by plasmin
Fibrinolysis can be of two types — primary fibrinolysis, which is the normal body process and secondary fibrinolysis, which is the breakdown of clots caused by a medicine, a medical disorder, or some other cause.
When blood clots are dissolved using medications to treat medical conditions, it is termed as thrombolysis.
After fibrinolysis/thrombolysis, the blood clot is removed, and the blood circulation continues as usual.
Hemostasis disorders
Malfunctioning of hemostasis leads to a bleeding disorder or clotting disorder. Disorders can be due to hypercoagulability (blood clots too much or too easily), hypocoagulability (not enough clotting), or iatrogenic coagulopathy (induced by medicines).
When the disorder is due to hypercoagulability or thrombophilia, it can cause:
- Deep vein thrombosis (DVT) — a blood clot in one’s leg or arm that can then travel to the lungs causing pulmonary embolism (PE), an obstruction of blood flow to that area of the lungs
- Stroke — a blood clot in the brain
- Myocardial infarction or heart attacks — due to a blood clot in the blood vessels of one’s heart
Thrombophilia occurs due to the interplay of both genetic and environmental factors. Genetic factors could be factor 5 Leiden mutation, protein C deficiency, protein S deficiency, prothrombin gene mutation, etc. Table 1 lists the genes that are associated with thrombophilia. Environmental factors could be oral contraceptive use; obesity; smoking; medical conditions like thyroid disorders, renal disease, abnormal liver function, cancer; surgery; etc.
Hypocoagulability can be caused by hemophilia, von Willebrand disease (deficiency of vWF), and inherited thrombocytopenia (low platelet count), which are genetic disorders. When one or more clotting factors are deficient or absent, the body cannot produce a clot at the injury site efficiently.
Signs and symptoms of a bleeding disorder7
- Blood in urine or stool
- Excessive bleeding that does not stop easily and may start spontaneously, such as with nosebleeds, or after a cut, dental procedure, or surgery
- Large bruises and bruising often
- Heavy bleeding after giving birth
- Heavy menstrual bleeding
- Petechiae, or bleeding under the skin causing tiny purple, red, or brown spots
- Redness, swelling, stiffness, or pain from bleeding into muscles or joints, which is particularly common with inherited hemophilia
- Umbilical stump bleeding that lasts longer than what is typical for newborns — about 1 to 2 weeks after the umbilical cord is cut — or that does not stop
Laboratory testing8,9,10
A wide range of tests of hemostasis are available — from routine coagulation assays to specialized hemostasis assays and platelet function. A summary of screening tests, clotting factor tests, and genetic tests follows.
Screening tests
The following is a list of screening tests to determine if the patient’s blood is clotting properly:
- Complete blood count (CBC) measures all blood components including platelets and can indicate presence of platelet disorder, if any.
- Prothrombin time (PT) measures the time it takes for blood to clot, primarily assessing the extrinsic pathway of the coagulation cascade. Normal PT values range from 9 to 13 seconds. Higher PT values indicate a prolonged clotting time, suggesting potential issues with clotting factors such as fibrinogen, factor V, VII, X, and prothrombin. Abnormal PT values may indicate liver disease, vitamin K deficiency, or the presence of anticoagulants.
- Partial thromboplastin time (PTT) measures the intrinsic and common pathways of the coagulation cascade, assessing factors such as VIII, IX, XI, and XII, as well as fibrinogen. Normal PTT values range from 25 to 35 seconds. Prolonged PTT may be due to deficiencies in these clotting factors, hemophilia, or the presence of inhibitors. Shortened PTT, may indicate an increased risk of thrombosis and could be associated with elevated factor VIII levels.
- Activated partial thromboplastin time (aPTT) measures the same coagulation factors as PTT with the addition of an activator, to make it clot faster.
- International normalized ratio (INR) is a standardized measure of PT, ensuring consistency in results across different laboratories. The normal range for INR is around 0.8 to 1.2. Higher INR values indicate a slower clotting time and an increased risk of bleeding. INR is particularly crucial for individuals on oral anticoagulants like warfarin.
- Fibrinogen test measures level of fibrinogen.
- D-Dimer is a marker for fibrin degradation products, indicating ongoing fibrinolysis. Normal D-dimer values are typically less than 500 ng/mL. Elevated D-dimer levels may be due to conditions such as deep vein thrombosis (DVT), pulmonary embolism (PE), disseminated intravascular coagulation (DIC), or other conditions associated with increased fibrin turnover. However, D-dimer is not specific, and elevated levels can also be seen in inflammation, infection, surgery, or pregnancy.
- A mixing test where the patient's plasma is mixed with an equal amount of normal plasma and tested to determine whether the clotting time prolongation is due to a coagulation factor deficiency or caused by antibodies blocking the clotting factors, such as with autoimmune disorders or acquired hemophilia.
Clotting factor tests
A clotting factor test measures the level or the activity of a specific clotting factor in the blood.8
- Von Willebrand factor (vWF) tests measure the amount of vWF in blood.
- Clotting factor VIII tests measure the activity of factor VIII in your blood. Very low levels of clotting factor VIII, may indicate hemophilia A.
- The Bethesda test looks for antibodies that may be blocking factor VIII or IX.
- Factor XIII antigen and activity assays assess factor XIII deficiency.
Genetic tests
FDA-approved molecular tests for factor II and factor V Leiden are available from a few manufacturers.
Quite a few clinical laboratories also offer comprehensive bleeding disorder panels using next-generation sequencing (NGS).
Treatment
Treatment depends on the type of the disorder. There are three general treatment options for bleeding disorders: risk reduction, medications (for example, antifibrinolytic agents, birth control pills, desmopressin, monoclonal antibodies, vitamin K supplements, etc.) and factor replacement therapy (For example: clotting factor concentrate, fresh frozen plasma, bypassing agents).11
Conclusion
Though a wide range of tests and treatment options, including gene therapy, are currently available, with the increasing use of artificial intelligence (AI) in healthcare and emergence of newer technologies like nanotechnology, we can hope to see use of AI in hemostasis. AI will enable more precise monitoring of coagulation and personalized medication for bleeding and clotting disorders, the development of novel hemostatic materials utilizing nanotechnology, and wider adoption of thromboelastography (TEG) for real-time assessment of blood clotting during surgery, which will facilitate better patient care by providing advanced diagnosis and treatment options for bleeding and thrombotic conditions.
References
- LaPelusa A, Dave HD. Physiology, hemostasis. In: StatPearls. StatPearls Publishing; 2025.
- Sokou R, Parastatidou S, Konstantinidi A, Tsantes AG, Iacovidou N, Piovani D. Stefanos Bonovas, Argirios E. Tsantes, Contemporary tools for evaluation of hemostasis in neonates. Where are we and where are we headed? Blood Reviews. 2024;64.
- Wilhelm G, Mertowska P, Mertowski S, et al. The crossroads of the coagulation system and the immune system: Interactions and connections. Int J Mol Sci. 2023;24(16):12563. doi:10.3390/ijms241612563.
- Chaudhry R, Usama SM, Babiker HM. Physiology, coagulation pathways. In: StatPearls. StatPearls Publishing; 2025.
- Chapin JC, Hajjar KA. Fibrinolysis and the control of blood coagulation. Blood Rev. 2015;29(1):17-24. doi:10.1016/j.blre.2014.09.003.
- Dautaj A, Krasi G, Bushati V, et al. Hereditary thrombophilia. Acta Biomed. 2019;90(10-S):44-46. doi:10.23750/abm.v90i10-S.8758.
- Bleeding Disorders Symptoms. NHLBI, NIH. Updated August 3, 2023. Accessed February 27, 2025. https://www.nhlbi.nih.gov/health/bleeding-disorders/symptoms.
- Bleeding Disorders Diagnosis. NHLBI, NIH. Updated August 3, 2023. Accessed February 27, 2025. https://www.nhlbi.nih.gov/health/bleeding-disorders/diagnosis.
- Zaidi SRH, Rout P. Interpretation of blood clotting studies and values (PT, PTT, aPTT, INR, anti-factor Xa, D-dimer). In: StatPearls. StatPearls Publishing; 2025.
- CDC. Diagnosing Hemophilia. May 15, 2024. Accessed February 27, 2025. https://www.cdc.gov/hemophilia/testing/index.html.
- Bleeding Disorders Treatment. NHLBI, NIH. Updated August 7, 2023. Accessed February 27, 2025. https://www.nhlbi.nih.gov/health/bleeding-disorders/treatment.
About the Author

Rajasri Chandra, MS, MBA
is a global marketing leader with expertise in managing upstream, downstream, strategic, tactical, traditional, and digital marketing in biotech, in vitro diagnostics, life sciences, and pharmaceutical industries. Raj is an orchestrator of go-to-market strategies driving complete product life cycle from ideation to commercialization.