Diagnostic marker found for deadly brain disease marked by dementia, movement problems
Researchers at Washington University School of Medicine in St. Louis have found a biomarker that identifies, with up to 89% accuracy, people with a primary tauopathy called corticobasal degeneration (CBD). Traditional diagnostic methods for CBD are only 25% to 50% accurate, the researchers said.
The biomarker could be developed into a tool to screen potential volunteers for CBD-specific research studies and clinical trials and, eventually, to identify people who could benefit from CBD-specific treatments, the scientists said.
The study was published November 24 in Nature Medicine.
In 2020, Kanta Horie, PhD, a research associate professor of neurology and the first author on the current paper, developed a highly sensitive technique to detect specific fragments of tau in the cerebrospinal fluid that surrounds the brain and spinal cord. Horie and colleagues used the technique to identify a novel form of tau in Alzheimer’s patients, and showed that the level of the novel tau in the cerebrospinal fluid indicates the stage of the disease, and tracks with the amount of tau tangles in the brain.
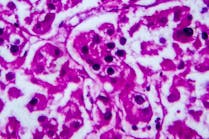
As part of this study, Horie, Sato and colleagues — including co-senior author Randall J. Bateman, MD, the Charles F. and Joanne Knight Distinguished Professor of Neurology — used the technique to search for distinctive forms of tau linked to primary tauopathies. To ensure that the study subjects were classified accurately, Horie, Sato and Bateman collaborated with co-authors Adam Boxer, MD, PhD, Salvatore Spina, MD, PhD, and Lawren VandeVrede, MD, PhD, all in the Department of Neurology at the University of California, San Francisco. The team examined brain tissues and cerebrospinal fluid from people who had died with dementia and movement disorders, and whose specific diseases had been confirmed at autopsy. The study population included people with one of five primary tauopathies — CBD; PSP; frontotemporal lobar degeneration with microtubule association protein tau mutations (FTLD-MAPT); agyrophilic grain disease; and Pick’s disease — as well as Alzheimer’s, and dementia not related to tau. For comparison, they also examined samples from people without dementia.
Two particular forms of tau — microtubule binding region (MTBR)-tau 275 and MTBR-tau 282 — were unusually high in the brains and low in the cerebrospinal fluid of patients with CBD and a subset of FTLD-MAPT. Further investigation showed that these forms of tau distinguish people with CBD from those with other primary tauopathies with 84% to 89% accuracy, depending on the disease.