Research has found that patients with COVID-19 are prone to serious blood clotting. However, a new study from Michigan Medicine found that aside from this heightened clotting risk, some COVID-19 patients have an unbalanced ability to break down clots as well, which is linked to a potential clinical biomarker seen in later stages of the disease, according to a news release from Michigan Medicine.
The study was published in Scientific Reports and led by senior author Daniel Lawrence, PhD, a Professor of Basic Research in Cardiovascular Medicine at Michigan Medicine.
The abnormal process of breaking down clots can contribute to a high bleeding risk, raising concerns about the current practice of giving COVID-19 patients high-dose anticoagulants throughout the duration of their disease course.
The Michigan study included 118 COVID-19 patients and 30 healthy controls. In the COVID-19 patients, the team expected to see high levels of plasminogen activator-inhibitor-1, a molecule associated with stabilizing blood clots. However, they did not expect high levels of tissue-type plasminogen activator, the molecule responsible for removing the clots.
According to the researchers, almost half of the study’s patients were supported by a ventilator and a quarter breathed just room air. Compared with the patients breathing room air, patients that required supplemental oxygen had significantly higher levels of plasminogen activator-inhibitor-1, but not of tissue-type plasminogen activator.
High levels of both tissue-type plasminogen activator (tPA) and plasminogen activator-inhibitor-1 (PAI-1) were associated with worse lung function, but high tPA independently correlated with mortality. The levels of either molecule can increase independently of one another, but the research also found a change in one can have consequences on the other.
The team asked whether COVID-19 plasma with the highest tPA levels might correlate with an enhanced, spontaneous breaking down of clots, as compared with low tPA COVID-19 plasma or control plasma.
After assessing 10 COVID-19 plasma samples with high tPA, 10 COVID-19 samples with low tPA and 10 healthy control plasma samples, it was clear the high-tPA COVID-19 samples were found to significantly enhance spontaneous clot breakdown compared to the other two groups. The researchers said this means that high tPA may be a biomarker for high bleeding risk and poorer outcomes in COVID-19.
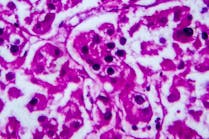
The researchers suspect the source of these high levels of tPA in COVID-19 patients, and the subsequent clotting issues, is because of damage to endothelial cells, which are cells that line blood vessels. If badly damaged, the blood vessels can actually break and cause bleeding.
The theory is that a hallmark symptom of COVID-19 ARDS, when fluid builds up in the lungs and causes trouble breathing and low oxygen levels in the blood, may trigger endothelial cell activation, which consequently promotes the release of tPA.