Biomarkers point to patients at higher risk for COVID-19 deterioration, death
George Washington University (GWU) researchers found five biomarkers, medical indicators found in the blood, associated with higher odds of clinical deterioration and death in COVID-19 patients, according to a press release from the university. The findings were published in Future Medicine.
“When we first started treating COVID-19 patients, we watched them get better or get worse, but we didn’t know why,” said Juan Reyes, MD, co-author of the study and assistant professor of medicine at the GW School of Medicine and Health Sciences. “Some initial studies had come out of China showing certain biomarkers were associated with bad outcomes. There was a desire to see if that was true for our patients here in the U.S.”
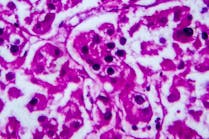
The research team evaluated 299 patients diagnosed with COVID-19 admitted to GW Hospital between March 12 and May 9, 2020. Of these patients, 200 had all five biomarkers being evaluated – IL-6, D-dimer, CRP, LDH and ferritin. Elevated levels of these biomarkers were associated with inflammation and bleeding disorder, showing an independent increased risk for ICU admission, invasive ventilatory support, and death. The highest odds of death occurred when the LDH level was greater than 1200 units/l and a D-dimer level was greater than 3 μg/ml.
Physicians often determine risk for COVID-19 deterioration and death based on age and certain underlying medical conditions, like having an immunocompromised state, obesity, and heart disease. Performing a simple blood test for patients admitted to the emergency department, then also making decisions based on biomarkers present, may further aid point-of-care clinical decision making.