A20 modulation: a potential biological threat that can be mitigated by immunohistochemistry
The views expressed in this publication/presentation are those of the author(s) and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the U.S. Government.
During the past two decades we have witnessed tremendous strides in the advancement of the biological sciences. In particular, molecular cloning has become a common activity, and the ability to develop genetically modified organisms has migrated from the confines of secure biological containment suites onto the open benches of undergraduate teaching labs.
Nowhere has this progress been more dramatic than in the fields of immunology and microbiology. Within a short period of time, our understanding of the immune system has been transformed from that of an intractable “black box” to an intricate series of networks in which a specific and defined set of signal transducing proteins control the initial activation and modulation of an expanding set of effector molecules, leading to outputs that are both predictable and tractable.1
Such progress has yielded an understanding of the mechanisms of disease at the molecular level and the ability to diagnose and treat both infectious and non-infectious ailments by rational means. However, detailed knowledge of the mechanisms of immunity can also be utilized to design specific and effective biological weapons, or to augment the capabilities of traditional biological threat agents.
Intentional biological attacks on the immune system
The vertebrate immune system has been under continuous selective pressure for approximately 500 million years.1 The architecture of this system can be divided into two distinct but interdependent branches: the innate and adaptive immune systems.
- The innate immune system uses germline-encoded receptors to detect pathogens via the recognition of a group of conserved constituents on the surface of invading microorganisms.
- The adaptive immune system is a complementary defense mechanism that utilizes gene rearrangement to form antigen receptors of nearly unlimited diversity, enabling the precise discrimination of self from non-self, the recognition of the majority of pathogens encountered throughout the life of the organism, and the constitution of an immunological memory.1
The age and complexity of the immune system, coupled with the high degree of diversity among the organisms with which it must contend, leads to the expectation that numerous genetic redundancies have accumulated over evolutionary time. However, research suggests that the necessary and sufficient functions of the immune system can be performed with a relatively small number of genes.2 The products of these genes are often targeted by pathogens, as a means of evading the host immune response, and it has been demonstrated that the modulation of these genes directly results in compromised immunity.2 These genes therefore represent critical vulnerabilities of the immune system, vulnerabilities that could potentially be exploited by adversaries through engineered biological weapons.
Currently, there are very few methods available to detect genetically engineered organisms or to rapidly respond to such a threat. It can be argued that the ability to manipulate biological systems has increased exponentially while the ability to detect these manipulations and develop effective countermeasures has increased linearly. This discordance has led to an environment in which it is possible to engineer a new biological threat agent in a matter of days, while the characterization of the threat and the development of countermeasures can take months to years.
A20 as a critical vulnerability of the immune system
Tumor necrosis factor alpha induced protein 3 or tnfaip3 is an example of a critical vulnerability of the immune system. Tnfaip3 encodes a 790-amino acid protein known as A20.3 A20 was initially identified in the early 1990s by a group working at the University of Michigan. This group was interested in the effects of a cellular mediator known as tumor necrosis factor alpha (TNF-alpha) on endothelial tissue.3 Their approach was to expose human endothelial cells to TNF-alpha, followed by molecular cloning of any gene products induced by this treatment. Several new proteins were identified, including A20. A20 expression was detected in nearly all tissues and all cell types, with high levels present in lymphoid tissue.
Further investigation revealed that the molecular activity of A20 involves the “editing” of ubiquitin chains.3 Ubiquitin is a small peptide which is covalently attached to substrate proteins as a monomer or multimer in one of several spatial conformations. Depending on the particular form of ubiquitin substitution, substrate proteins are targeted for either degradation or functional modification.3 Through these ubiquitin editing activities, A20 has the potential to modulate the activity of a broad range of intracellular signal transducers.
Recently, a group working at the University of California in San Francisco showed that A20 plays a crucial role in the immune system. Their studies employed a “knock-out” mouse model in which the gene encoding A20 was inactivated in the mouse genome.3 The resulting mouse strain was evaluated for defects resulting from this deletion. The results of these studies showed that A20 knock-out mice exhibit systemic multi-organ inflammation, in response to commensal flora, leading to early death. Interestingly, if these mice were given large doses of antibiotics, systemic inflammation was reduced and the mice survived.3 This result suggested that A20 holds immune responses in check, as the absence of A20 leads to an exaggerated and ultimately fatal immune response to non-pathogenic commensal bacteria.
Later studies revealed that A20 plays a key role in limiting the extent of both innate and adaptive immune responses. It has been shown that A20 is directly involved in regulating both the morbidity and mortality resulting from acute viral infection and intracellular parasitemia.4 In 2012, a Belgian group reported that the deletion of A20 in myeloid cells protects mice from lung damage during mild influenza A virus infection. Myeloid-specific A20 knock-out mice are also protected from the mortality resulting from a lethal dose of influenza A virus.4 This study demonstrates that A20 is indeed a central gatekeeper of the immune response, since the deletion of this gene alone is able to alter the outcome of a viral infection.
The central role of A20 has been exploited by various groups of pathogens to evade the host immune response. For example, the measles P protein has been shown to upregulate the expression of A20 as a means of dampening the innate immune response, and a group working in India reported that the protozoan parasite Leishmania donovani has evolved a mechanism for modulating A20 activity as a means of facilitating intracellular survival.5
A20 is also a target for biological toxins. There is data to suggest that A20 is involved in maintenance of epithelial barriers and in the destruction of allergens and toxins via an intracellular degradation pathway involving vesicles called endosomes and lysosomes.6 It has been shown that cholera toxin forms complexes with A20 in the cytoplasm. Cholera toxin sequestration inactivates A20, preventing interaction with substrate molecules.6 The end result is that cholera toxin-mediated inhibition of A20 leads to the breakdown of epithelial barriers, with the concomitant release of allergens and toxins into the cytosol.
Modulation of A20 as a biological threat
The fact that A20 plays a critical and non-redundant role in the immune response to bacterial, viral, and protozoan pathogens makes this molecule an attractive target for biological weapons development. There are several means by which the activity of A20 could be modulated by a biological weapons designer. The most likely method would be to genetically modify a traditional biological agent or an emerging pathogen to interfere with the activity of A20 in such a way as to enhance pathogen virulence. For example, Bacillus anthracis could be engineered to deliver an A20-activating enzyme, together with chromosome-encoded protective antigen and edema factors. Since A20 down-regulates both the innate and adaptive immune systems, the activation of A20 in the context of an anthrax infection could enable the pathogen to escape the immune response, thereby increasing virulence. In addition, this strategy might allow a smaller number of spores to initiate infection, increasing the efficiency of either line-source or point-source dissemination.
Another possible scenario is that anthrax and cholera toxin could be delivered simultaneously as a binary weapon.6 Complex formation between cholera toxin and A20 would lead to a breakdown in epithelial barriers, causing increased spread of anthrax and anthrax-associated toxins resulting in increased virulence. Similarly, a viral pathogen such as influenza could be engineered to express an A20-degrading enzyme. This modification may have the effect of exacerbating the immune response to the virus in the upper respiratory tract, leading to increased pathology. The technology to modify Bacillus anthracis and the influenza virus not only exists, but is widespread. A20 is being actively researched on at least three continents. Thus, there is potential for the diffusion of technical knowledge regarding A20 and its properties to potential adversaries.
A20 as a biomarker in detecting malevolent biological engineering
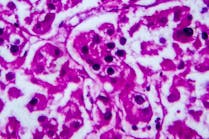
Although A20 analysis is not currently performed in the clinical setting, it is an emerging biomarker with the potential to augment the analysis of novel (engineered) host-pathogen interaction. Since the clinical laboratory is essential to the detection of unusual pathogens in the patient population, this may be the ideal environment for the detection of overt A20 modulation. While there are several methods which can be used to monitor A20 activity, immunohistochemistry is the most attractive. This is due to the fact that immunohistochemistry allows direct visualization of the protein and requires no prior knowledge of how A20 modulation may have been achieved. Normally A20 tends to localize into discrete punctate structures in the cytoplasm.7 These structures have been visualized with the aid of fluorescently-tagged antibodies. Such antibodies can be used to determine whether A20 is present in clinical samples, whether it is under-expressed or over-expressed, and possibly to determine whether it is properly localized. In addition, antibodies can be developed to target individual A20 domains. This will make it possible to determine whether an organism is expressing a specific domain, if a specific domain from endogenous A20 has been re-targeted, or whether A20 has been cleaved by an anti-A20 enzyme resulting in a separation of the domains.
Conclusion
As technology advances and our knowledge regarding the molecular mechanisms underlying the delicate interaction between bacterial and viral pathogens and the host immune response becomes more sophisticated, the possibility of the malevolent application of this knowledge will also increase. The clinical laboratory staff is on the frontlines of biodefense and will undoubtedly play an important role in the detection and response to future biological threats, whether natural or manmade. In order to be prepared for novel threats, it is essential that laboratory staff have a thorough understanding of what is possible and are provided with the tools to respond to unusual and novel situations. The methods of immunohistochemistry and the application of fluorescently tagged antibodies are uniquely suited to this task since they can be utilized in a hypothesis-free manner and to rapidly generate the data which may be used to identify the mechanism of action of an engineered agent. While many intracellular signaling molecules have been described, A20 is unique in that it appears to be a central regulator of the immune response and is thus a logical target for both natural as well as man-made biological agents. It is therefore essential that laboratory personnel be familiar with A20 and that the specific reagents be prepared to monitor its activity.
References
- Flajnik MF, Kasahara M. Origin and evolution of the adaptive immune system:
genetic events and selective pressures. Nature Reviews Genetics. 2010;11(1):47-59. - Janeway CA, Travers P, Walpor MJ, Shlomchik MJ. Immunobiology: the immune system in health and disease (Vol. 2). 2001. London: Churchill Livingstone.
- Verstrepen L, Verhelst K, van Loo G, Carpentier I, Ley SC, Beyaert R. Expression, biological activities and mechanisms of action of A20 (TNFAIP3). Biochem Pharm. 2010; 80(12):2009-2020.
- Maelfait J, Roose K, Bogaert P, et al. A20 (Tnfaip3) Deficiency in myeloid cells
protects against influenza A virus infection. PLOS Pathog. 2012;8(3):e1002570. doi:10.1371/journal.ppat.1002570. - Srivastave S, Kar S, Chande AG, Mukhopadhyaya R, Das PK. Leishmania donovani exploits host deubiquitinating enzyme A20, a negative regulator of TLR signaling, to
subvert host immune response. J. Immunol. 2012;189: 924-934. - Li MY, Zhu M, Zhu B, Wang ZQ: Cholera toxin suppresses expression of ubiquitin editing enzyme A20 and enhances transcytosis. Cell Physiol Biochem. 2013;31:495-504.
- Li L, Hailey DW, Soetandyo N, et al. Localization of A20 to a lysosome-associated compartment and its role in NFқB signaling. Biochimica et Biophysica Acta (BBA) Molecular Cell Research. 2008;1783.6:1140-1149.
Maj. Michael A. Washington, PhD, M(ASCP), serves as the Chief of Microbiology Research in the Department of Clinical Investigation at Tripler Army Medical Center in Honolulu, HI. He is currently engaged in research designed to improve the ability of the U.S. military to identify and respond to biological threats.