Sepsis: Definition, diagnosis, and management
Sepsis is a systemic inflammatory reaction mainly caused by pathogen infection, which is often characterized by high fever, leukocytosis, and headache.1 Sepsis can lead to multiple organ dysfunction syndrome (MODS) and circulatory failure in critical condition. In 2016, The European Society of Intensive Care Medicine (ESICM) and the Society of Critical Care Medicine (SCCM) defined sepsis as a life-threatening organ dysfunction caused by a dysregulated host response to infection.2 The body’s reaction causes damage to its own tissues and organs leading to septic shock, multiple organ failure, and sometimes death, if not recognized early and treated promptly. The Centers for Disease Control and Prevention (CDC) reports that at least 1.7 million adults develop sepsis annually in U.S. hospitals and at least 350,000 adults who develop sepsis die during their hospitalization or are discharged to hospice.3
Sepsis is usually caused by bacterial infections but infections from viruses such as COVID-19 and influenza, parasites or fungi, or noninfectious insults, such as traumatic injury, can also cause sepsis.3 Normally, to combat the infection or traumatic insult, the body releases chemical or protein immune mediators into the blood. If unchecked, those immune mediators trigger widespread inflammation, blood clots, and leaky blood vessels, causing impaired blood flow and organs becoming deprived of nutrients and oxygen, which leads to organ damage.4 The bacteria that have been predominantly found to be responsible for sepsis and septic shock are Gram-positive bacteria — Staphylococcus aureus and Streptococcus pneumoniae and Gram-negative bacteria — Escherichia coli, Klebsiella, and Pseudomonas spp.5 Previously, it was believed that Gram-negative bacteria was the major cause of sepsis and septic shock;6 however, presently, it has been shown that Gram-positive bacteria are the predominant cause of sepsis and septic shock.4,6 Among fungi, Candida species are predominantly responsible for causing sepsis and septic shock in immunosuppressed or neoplastic patients undergoing long-term treatment with chemotherapeutic and immunosuppressive drugs.8
The pathogenic Gram-positive and Gram-negative bacteria produce different types of toxins. Toxins from the bacteria helps the pathogenic bacteria to modulate host defenses, enabling them to escape the innate immune system to remote organs resulting in sepsis or septic shock. The outcome of the disease depends on the type of the toxin.9 Infection in sites that may lead to sepsis and their percent of occurrence are as follows: 8,10
- Respiratory tract/pulmonary parenchyma (43%)
- Urinary system (16%)
- Abdomen (14%)
- Head, which is associated with a fever of unknown origin (14%)
- Other sites/causes (13%)
People at high risk
The people who are at high risk of sepsis are the following: 11
- People older than 65 years old, newborns and infants, and pregnant women
- People having medical conditions such as diabetes, obesity, cancer, and kidney disease
- People with weakened immune systems
- People who are in the hospital for other medical reasons
- People with severe injuries, such as large burns or wounds
- People with catheters, IVs, or breathing tubes
- People with certain genetic variants are more prone to sepsis12
Stages of sepsis
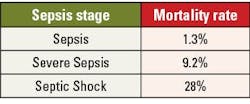
There are three stages of sepsis: sepsis, severe sepsis, and septic shock.11
In the first stage, the immune response overreacts to an infection or injury resulting in a situation like systemic inflammatory response syndrome. However, at this stage it is very difficult to diagnose sepsis.
A patient having sepsis may have one or more of the following signs or symptoms: 2
- Clammy or sweaty skin
- Confusion or disorientation
- Extreme pain or discomfort
- Fever, shivering, or feeling very cold
- High heart rate or weak pulse
- Shortness of breath
Severe sepsis occurs when acute organ dysfunction begins and there is failure of one or more organs. Symptoms of severe sepsis are as follows:13
- Changes in skin color or patches of discolored skin
- Low or no urine output
- Disorientation, drowsiness, changes in mental ability, loss of consciousness
- Difficulty breathing
- Abnormal heartbeat
- Chills
- Extreme weakness
Septic shock is a serious condition that occurs when a body-wide infection leads to dangerously low blood pressure. Septic shock can affect any part of the body, including the heart, brain, kidneys, liver, and intestines. Symptoms of septic shock are as follows: 14
- Cool, pale arms and legs
- High or very low temperature, chills
- Lightheadedness
- Little or no urine
- Low blood pressure, especially when standing
- Palpitations
- Rapid heart rate
- Restlessness, agitation, lethargy, or confusion
- Shortness of breath
- Skin rash or discoloration
- Decreased mental status and confusion
For the mortality rate in sepsis stages, see Table 1.
Diagnosis of sepsis
At present, there is not a single test to identify sepsis. Thus, doctors and healthcare professionals use a combination of tests and clinical signs to diagnose sepsis.16 Broadly, these tests determine the following:16
- The presence of an infection, if any. If detected, identify the organism and determine antibiotic susceptibility
- Very low blood pressure and high heart rate
- Increased breathing rate
- Urinary tract infections (UTI) or kidney problems
- If the immune system has gone into an over-reactive mode using certain blood tests
Because sepsis is highly complex and can progress to multiple organ dysfunction syndrome and death, various tools are used that incorporate clinical evaluation, vital signs, and laboratory results to screen, recognize severity, risk stratification prognosis and mortality. Some tools that have been used for this purpose are:
- Systemic Inflammatory Response Syndrome (SIRS) criteria,
- Quick Sequential Organ Failure Score (qSOFA),
- Sequential Organ Failure Assessment (SOFA) criteria,
- National Early Warning Score (NEWS), and
- Modified Early Warning Score (MEWS).17
The laboratory tests conducted for patients suspected of having sepsis are:18
- Complete blood count, including white blood count and platelet count
- Serum creatinine
- Bilirubin
- Serum lactate
- Procalcitonin (PCT)
- C-reactive protein (CRP)
- Urinalysis
- Blood culture followed by identification and antibiotic susceptibility testing if bacteria is detected
If viral or fungal infection is suspected, appropriate specimens need to be collected for their detection.
Genetic markers for sepsis
Studies are being carried out to understand the occurrence and progress mechanism of sepsis at the genomic level and provide new targets for clinical diagnosis and treatment of sepsis. Studies have identified a few potential biomarkers markers of sepsis, such as ITK, CD247, MMP9, CD3D, MMP8, KLRK1, and GZMK.19 However, genetic test for sepsis are still not in practice.
That said, rapid and sensitive molecular tests are often used to detect if there is any infection.
Management and treatment of sepsis
As sepsis and septic shock are medical emergencies, early identification and treatment initiation improve outcomes in sepsis patients. These patients need constant monitoring and are often monitored and treated in ICUs. The treatment for septic and septic shock patients are as follows:5
First pillar of sepsis/septic shock treatment — antimicrobial therapy to control infection
To control the infection, antimicrobial therapy needs to be initiated immediately, ideally within one hour after admission. Microbiological specimens — blood, fluid or tissue from sites based on the clinical evaluation — need to be collected and analyzed as soon as possible for identification of infection. The choice of initial empiric antimicrobial therapy is based on clinical (i.e., site of infection, previous antibiotic use, immunosuppression, and risk factors for resistant organisms) and epidemiological criteria.
For patients proceeding toward septic shock, multidrug antimicrobial regimens with a wide spectrum of activity should be used (e.g., carbapenems and anti-Gram-negative antimicrobials with dual coverage). Dual coverage for Gram-negative organisms might be appropriate in cases of high suspicion for multidrug-resistant organisms (e.g., Pseudomonas aeruginosa or Acinetobacter baumanii). Dual coverage for Gram-positive organisms and methicillin-resistant Staphylococcus aureus (MRSA) should be considered for patients with a high risk of infection due to these pathogens.
The second pillar of treatment – intravenous fluid resuscitation
Intravenous fluid helps to increase depleted or functionally reduced intravascular volume that occurs in sepsis owing to vasodilated vascular network. Balanced crystalloids have been the fluid of choice with continuous hemodynamic monitoring to avoid fluid overload.
The third pillar of treatment – vasoactive agents
To maintain mean arterial pressure above 65 mmHg and reduce the risk of fluid overload vasoactive drugs are administered. Norepinephrine (NE) has been the first line of choice. Vasopressin (VP) and Epinephrine may be considered as second and third lines of treatment respectively for septic shock.
Oxygen and ventilation support
Patients may require oxygen or ventilation support, for example, when blood oxygen levels are low or the patient has sepsis-induced acute respiratory distress syndrome (ARDS).
Other treatment
Based on the clinical condition of the patient, it may be required to administer other medications to the patients including heparin, insulin, steroid, acetaminophen etc.
Conclusion
Sepsis is a very complex and challenging syndrome as it extends beyond the infection type and encompasses a spectrum of biological processes, including inflammation, coagulation, endothelial activation, and alterations in the microbiome.20, 21
Even though at present it is not possible to confirm sepsis and predict the prognosis using one single test, with the advancements in omics technologies (genomics, transcriptomics, proteomics, metabolomics, cytomics) coupled with artificial intelligence and machine learning, we can hope to detect sepsis, predict prognosis, and recommend personalized therapy to patients with sepsis in the future.
References
- Evans L., Rhodes A., Alhazzani W., et al. Executive summary: Surviving sepsis campaign: International guidelines for the management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):1974-1982. doi:10.1097/CCM.0000000000005357.
- Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801. doi:10.1001/jama.2016.0287.
- CDC. About. Sepsis. Published May 13, 2024. Accessed September 25, 2024. https://www.cdc.gov/sepsis/about/?CDC_AAref_Val=https://www.cdc.gov/sepsis/what-is-sepsis.html.
- National institute of general medical sciences. National Institute of General Medical Sciences (NIGMS). Accessed September 25, 2024. https://www.nigms.nih.gov/education/fact-sheets/Pages/sepsis.aspx?ref=prendi-il-controllo-della-tua-salute.com.
- Guarino M, Perna B, Cesaro AE, et al. 2023 update on sepsis and septic shock in adult patients: Management in the emergency department. J Clin Med. 2023;12(9):3188. doi:10.3390/jcm12093188.
- Parrillo JE, Parker MM, Natanson C, et al. Septic shock in humans. Advances in the understanding of pathogenesis, cardiovascular dysfunction, and therapy. Ann Intern Med. 1990;113(3):227-42. doi:10.7326/0003-4819-113-3-227.
- Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54. doi:10.1056/NEJMoa022139.
- Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(21):2063. doi:10.1056/NEJMc1312359.
- Ramachandran G. Gram-positive and gram-negative bacterial toxins in sepsis: a brief review. Virulence. 2014;5(1):213-8. doi:10.4161/viru.27024.
- Vakkalanka J.P., Harland K.K., Swanson M.B., Mohr N.M. Clinical and epidemiological variability in severe sepsis: An ecological study. J Epidemiol Community Health. 2018;72:741–745. doi:10.1136/jech-2018-210501.
- Cleveland Clinic. Sepsis. Accessed September 25, 2024. https://my.clevelandclinic.org/health/diseases/12361-sepsis.
- Engoren M, Jewell ES, Douville N, Moser S, Maile MD, Bauer ME. Genetic variants associated with sepsis. PLoS One. 2022;17(3):e0265052. doi:10.1371/journal.pone.0265052.
- Sepsis Alliance. Severe Sepsis. Published November 11, 2019. Accessed September 25, 2024. https://www.sepsis.org/sepsis-basics/what-is-sepsis/severe-sepsis/.
- MedlinePlus. Septic shock. Bethesda, MD: National Library of Medicine (US); Updated November 23, 2023. Accessed September 2024. Available from: https://medlineplus.gov/septicshock.
- Shapiro N, Howell MD, Bates DW, Angus DC, Ngo L, Talmor D. The association of sepsis syndrome and organ dysfunction with mortality in emergency department patients with suspected infection. Ann Emerg Med. 2006;48(5):583-90, 590.e1. doi:10.1016/j.annemergmed.2006.07.007.
- Sepsis. Yale Medicine. Published October 29, 2022. Accessed September 25, 2024. https://www.yalemedicine.org/conditions/sepsis.
- Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-1247. doi:10.1007/s00134-021-06506-y.
- Fulton MR II, Zubair M, Taghavi S. Laboratory evaluation of sepsis. In: StatPearls. StatPearls Publishing; 2024.
- Liang J, Wu W, Wang X, Wu W, Chen S, Jiang M. Analysis of sepsis markers and pathogenesis based on gene differential expression and protein interaction network. J Healthc Eng. 2022;12;2022:6878495. doi:10.1155/2022/6878495.
- van der Poll T, Shankar-Hari M, Wiersinga WJ. The immunology of sepsis. Immunity. 2021;9;54(11):2450-2464. doi:10.1016/j.immuni.2021.10.012.
- van der Poll T, van de Veerdonk FL, Scicluna BP, Netea MG. The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol. 2017;17(7):407-420. doi:10.1038/nri.2017.36.
About the Author

Rajasri Chandra, MS, MBA
is a global marketing leader with expertise in managing upstream, downstream, strategic, tactical, traditional, and digital marketing in biotech, in vitro diagnostics, life sciences, and pharmaceutical industries. Raj is an orchestrator of go-to-market strategies driving complete product life cycle from ideation to commercialization.