It’s personal: the evolution of respiratory diagnostics
Respiratory diagnostics is complicated, especially lately. The COVID-19 pandemic sparked innovation, and for the past few years manufacturers have flooded the market with new options for respiratory diagnostics. As the diagnostic landscape continues to evolve, and with so many variables at play, the laboratorians and clinicians I meet across the country are asking some important questions about the optimal solutions for their institutions. They’re also looking at how diagnostic stewardship applies to each option, which makes decision-making even more challenging.
A roadmap for diagnostic testing
To optimize a respiratory testing strategy — and algorithm — that leads to the best patient outcomes, it’s important to consider several factors, including patient setting, risk stratification, and impact to patient management. Navigating all these factors is a major challenge for health networks; there really is no “one-size-fits-all” solution. Diverse care settings and patient populations require different types of tests. There are also issues of workflow, timing, quality, managing ordering and inventory, and aligning stakeholders.
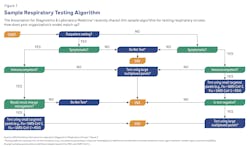
Fortunately, there are models that can provide a roadmap. The Association for Diagnostics and Laboratory Medicine (ADLM), for example, has published a guidance document on laboratory diagnosis of respiratory viruses that includes a suggested testing algorithm1 (see Figure 1). Additionally, when institutions share algorithms and best practices, it benefits everyone and enhances diagnostic stewardship.
In this article, which focuses on polymerase chain reaction (PCR) respiratory testing ,2 we will follow the journey of one institution, Vanderbilt Health, to understand how its laboratorians and care providers approached the challenges of creating and revising both inpatient and outpatient testing algorithms for respiratory viruses in the post-pandemic era.3
A hodgepodge of options
The ADLM recommends PCR testing because of its sensitivity and specificity, and because of PCR testing’s potential for automation, which is particularly useful in high-volume settings, reducing contamination risk and hands-on time required by staff.1
PCR-based diagnostics are just one slice of the diagnostic pie, and PCR testing is a rich, complex slice. There are dozens of options to choose from in a variety of configurations, including singleplex (one pathogen), targeted multiplex (2–5 pathogens) and expanded multiplex (6+ pathogens). These options are further categorized by their complexity as it relates to Clinical Laboratory Improvement Amendments (CLIA), allowing them to either be performed at the point of care or in central labs. With so many options available, how can institutions determine how best to position these technologies to meet the needs of their diverse patient populations?
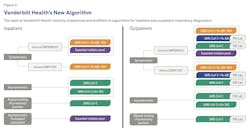
Vanderbilt Health operates seven hospitals and more than 200 clinics in the southeastern United States, and recently overhauled its algorithms for inpatient and outpatient testing (see Figure 2). It offers a variety of PCR testing options to suit the many providers in its system. However, in recent years that variety has swelled into “a bit of a hodgepodge,” according to David Gaston, MD, PhD, medical director of Vanderbilt Health’s Molecular Infectious Disease Laboratory (MIDL).3
“Everything was SARS-CoV-2 for a solid two years,” Gaston said. “The algorithm was built and then it expanded. Then the lab would bring in new technologies and new testing panels, and it would expand more.”3
It was time for a reset — and a more focused testing panel.
Streamlining the system
According to the ADLM, selection of the right test involves evaluation of test performance, testing volume, laboratory feasibility, cost versus value and the overall impact on clinical outcomes.1 Sometimes, selecting the right test requires rethinking existing algorithms.4
When Vanderbilt Health transitioned to a new and expanded off-site laboratory, the move created an opportunity to revamp the lab’s information systems and revise its testing algorithms. “The question was how to take some of the testing that had gotten away from a diagnostic stewardship focus and align it while we had the ear of the hospital and a lot of providers,” Gaston said.
Close examination of data revealed that “SARS-CoV-2 was still relevant, but less so, and influenza A was very prominent, as was RSV (respiratory syncytial virus),” Gaston said. “Showing providers that data was very compelling. It implied that perhaps broad respiratory testing for all patients wasn’t needed.”
The transformation at Vanderbilt also gave the clinical side a chance to step back and ask if they were meeting patient needs as efficiently as possible. “That was a big part of the success of [developing our new algorithm],” said Alisha Ezell, MHA, MLS (ASCP)CM, Vanderbilt Health’s enterprise point-of-care manager for diagnostic laboratories. “It was a chance to integrate MIDL’s perspective and have point of care come together with our physicians to determine if we were making changes that made sense for the entirety of our patient care and all the patients that we serve.”
After years of experience dealing with the pandemic, the Vanderbilt Health team set out to create algorithms that were more sensitive, nuanced, and precise. Another change was to move away from the focus on point-of-care testing to “bringing as much as possible back to the lab” to allow providers and clinicians to focus on patients.
A listening tour
Key principles of diagnostic stewardship noted by the Society for Healthcare Epidemiology of America (SHEA)5 include multidisciplinary collaboration and including all workers affected by steps in the diagnostic pathway.5 Vanderbilt Health’s transformation is a strong example of following these practices, which improved the finished product while also making the people who were consulted feel more invested in, and receptive to, the new algorithm.
To reach that end, Gaston made sure that everyone even remotely impacted by the algorithm revision had a seat at the table. He sent “cold call” emails to myriad departments, including OB/GYN, emergency medical, and acute care oncology, asking for their thoughts on the algorithm revision. “We wanted to pull as many of those perspectives together as possible and find something that was flexible enough so that anyone could use it and not encounter roadblocks and restrictions,” he said.
Meanwhile, Ezell spent time determining who all of the stakeholders might be. “It starts with the clinicians and what they’re seeing and what impact the algorithm will have on them when we change it,” she said. “Boots on the ground” frontline medical workers need a voice, too. “Sometimes we forget that our nurses are right there with the patients, and that changes we make to the algorithm are going to impact their workflows,” she said. “We don’t want to make it harder for them to do their jobs. If we pull them away to do more work to get lab results, then we’re pulling them away from their patients.”
Building a better algorithm
For algorithms to be of use, they need to “be in line with institutional standards but also flexible enough for providers to pursue different testing routes,” Gaston said. “I’ve had lots of conversations with providers where I’ve said, ‘I never would have thought of that use case. Let’s go back to the drawing board and figure out how we can fit this in and make it work.’”
To create new inpatient and outpatient respiratory testing algorithms for Vanderbilt Health (see Figure 2), Gaston and his team aligned their testing strategy with institutional goals set by multidisciplinary teams. They established that fourplex testing for SARS-CoV-2, RSV, influenza A, and influenza B should be the first step. “That’s really where I think most people should start,” he said.
Seasonality wasn’t a factor. “At this moment we’re not changing based on the respiratory season because we haven’t had a normal respiratory season for the past four years,” Gaston said.
As SHEA emphasizes, the way providers order tests is an important part of the equation because it allows for numerous interventions to improve test utilization.5
Gaston started with fourplex because “there’s been a lot of flu,” and that option is preselected in the test order set. For inpatients, all contact precautions are preselected and contacts with infection prevention are all automated, so the provider doesn’t have to click through a long list of selections.
“We’ve found that many providers would open the order set and just click ‘order,’” Gaston said. “So when a broad multiplex panel is the first thing that comes up, that will be what’s ordered. That might be what the provider wants, but it might not be.”
Gaston wants to make it as easy as possible to order the test that the lab thinks will have the most clinical value for the greater population. The fourplex is at the top of the list so that the clinicians have a higher likelihood of selecting that without having to put a lot of thought into it.
“We’re not forcing them to make that selection,” Gaston said. “The provider just has to search a bit harder to find broader multiplex options.”
Changing the algorithms, including the way that tests are presented in the order panel, has made a positive impact throughout the Vanderbilt Health system, Gaston said: “We’ve gotten great feedback from providers, who are very much engaged and see this as something to which they want to contribute.”
The system is more efficient too. Changing from the previous respiratory algorithm to the current one has decreased clicks by anywhere from three to five, Gaston said. “For providers, that matters a lot.”
REFERENCES
- Berry GJ, Jhaveri TA, Larkin PMK, Mostafa H, Babady NE. ADLM guidance document on laboratory diagnosis of respiratory viruses. J Appl Lab Med. 2024;2;9(3):599-628. doi:10.1093/jalm/jfae010.
- Walter JM, Wunderink RG. Severe respiratory viral infections: New evidence and changing paradigms. Infect Dis Clin North Am. 2017;31(3):455-474. doi:10.1016/j.idc.2017.05.004.
- Gaston DC, Ezell A. Advancing respiratory testing across the continuum of care. In: Presented at: ADLM Annual Scientific Meeting & Clinical Lab Expo; Roche Idea Lab. ; 2024.
- Schinas G, Dimopoulos G, Akinosoglou K. Understanding and implementing diagnostic stewardship: A guide for resident physicians in the era of antimicrobial resistance. Microorganisms. 2023;11(9):2214. doi:10.3390/microorganisms11092214.
- Fabre V, Davis A, Diekema DJ, et al. Principles of diagnostic stewardship: A practical guide from the Society for Healthcare Epidemiology of America Diagnostic Stewardship Task Force. Infect Control Hosp Epidemiol. 2023;44(2):178-185. doi:10.1017/ice.2023.5.
- Vicente AM, Ballensiefen W, Jönsson JI. How personalised medicine will transform healthcare by 2030: the ICPerMed vision. J Transl Med. 2020;28;18(1):180. doi:10.1186/s12967-020-02316-w.
The future will be flexible
Vanderbilt Health’s new respiratory algorithms were built with flexibility in mind because flexibility is a key factor in providing the right test for the right patient at the right time. In the future, as personalized medicine continues to transform healthcare, we expect to see new types of diagnostic tests, including tests that are faster, more customizable, and more aligned with principles of diagnostic stewardship.6 These increasingly more flexible tests have the potential to improve workflow, minimize costs, and overcome reimbursement obstacles.
About the Author

Alesia McKeown, PhD
is a Scientific Partner for Infectious Disease in Medical and Scientific Affairs at Roche Diagnostics. She is the subject matter expert for Roche’s high-throughput and POC respiratory solutions. She also co-leads an interdisciplinary team focused on improving access and utilization of diagnostics in the respiratory disease area.