Diabetes: The current state of affairs from a population management view
CONTINUING EDUCATION
To earn CEUs, visit www.mlo-online.com under the CE Tests tab.LEARNING OBJECTIVES
1. List factors that are important in controlling the at-risk management of diabetes.
2. Describe symptoms, causes, and complications of various types of diabetes.
3. Describe trends, statistics, and healthcare cost dilemmas in regard to diabetes.
4. Discuss programs that have led to standardization and improvement among a variety of HbA1c testing methods and the outcomes.
The Affordable Care Act and population management have significantly changed how diabetes screening is viewed. In today’s preventive care environment, healthcare providers understand that staying ahead of the progression of the disease and associated comorbidities, minimizing the financial implications of disease progression, and improving patient outcomes and quality of life are dependent on the proactive screening for and management of at-risk patients. Laboratory and point-of-care testing (POCT), therefore, play a critical role and bring significant value in the screening, monitoring, and management of these patients. In this article, we will review the physiological implications of diabetes, risk factors, and importance of population management. We will conclude with an overview of the current practices for screening, diagnosis, and monitoring and how the laboratory and POCT add value in the context of healthcare reform initiatives.
Physiologically, the condition of diabetes (diabetes mellitus) is characterized by elevated blood glucose or hyperglycemia, primarily driven by the deficiency of insulin production in the beta cells of the pancreatic islets or the inability of cells to respond to insulin that is produced.1,2 Elevated blood glucose is often accompanied by symptoms that include frequent urination and increased thirst and hunger. If the diabetes goes undiagnosed and untreated, short term, acute complications include diabetic ketoacidosis and hyperglycemic coma. However, the severity, complexity, and mortality of long-term complications of diabetes are of most concern from a chronic disease or population management perspective. These conditions include chronic kidney failure, cardiovascular disease, stroke, ulcerations and wounds in the lower extremities, and eye diseases including cataracts, retinopathy, and glaucoma.3,4
The National Diabetes Statistics Report (2014) from the Centers for Disease Control and Prevention (CDC) lasers in on the ever-increasing burden of diabetes. A key statistic to note is the estimated 9.3 percent of the population of the United States—29.1 million individuals—who have diabetes.5 Of those individuals, 21 million have been diagnosed, but more than eight million remain undiagnosed and therefore untreated. In 2012, diabetes and its related complications accounted for $245 billion in total medical costs and lost work and wages. This figure is up from $174 billion in 2007.5
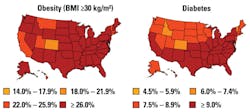
The estimated number of individuals 20 years of age or older who are pre-diabetic is 86 million, versus 79 million in 2011, with these individuals being at increased risk of developing multiple chronic diseases and conditions over their lifetime.5 Indeed, the prevalence of pre-diabetes, diabetes, and associated chronic diseases has doubled over the past two decades, primarily as a result of the burden of obesity across the U.S. (Figure 1).6
Types of diabetes
Type 1 diabetes was previously called insulin-dependent diabetes mellitus or juvenile-onset diabetes. Although disease onset can occur at any age, most cases are diagnosed in patients’ mid-teens. In a type 1 diabetic individual, the body’s immune system has attacked and destroyed the beta cells, incapacitating the pancreas’s ability to make the amount of insulin needed to moderate glucose levels in the body.
There is no way to prevent the onset of type 1 diabetes, but the disease is manageable. Treatment for type 1 diabetes includes administration of insulin by injection, pump, or orally; appropriate diet and exercise; and monitoring and control of blood pressure and lipid levels.5,7
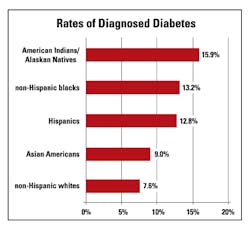
Type 2 diabetes, which used to be called adult-onset diabetes, can affect individuals of all ages, but onset is most often seen in middle-aged and older individuals. The risk for developing disease increases among individuals who are overweight and inactive. Increased prevalence of diabetes is also seen among specific ethnic groups such as African Americans, Hispanics, and Native Americans, as well as among lower socio-economic groups in certain geographical regions of the U.S. (Figure 2).5,7,8
Type 2 diabetes usually begins with insulin resistance—a condition that occurs when fat, muscle, and liver cells do not use insulin to carry glucose into the body’s cells to use for energy.1,6 As a result, the body needs more insulin to help glucose enter cells. Initially, the beta cells of the pancreas will produce more insulin to manage the added demand. But eventually the pancreas is no longer able to produce sufficient insulin when blood sugar levels increase, such as after meals.6,9 At this point, type 2 diabetes has ensued.
Treatment for type 2 diabetes includes use of diabetes medications, dietary changes, and increased physical activity (as diet and lack of exercise are recognized as high-risk factors for developing type 2 diabetes), along with the monitoring and control of blood pressure and lipid levels.5,7
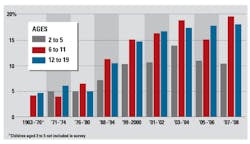
An alarming trend across the U.S. is the increasing incidence of type 2 diabetes among individuals < 20 years of age (Figure 3). Additionally, the SEARCH for Diabetes in Youth study (SEARCH) estimated that in 2001 about 154,000 individuals in the U.S. aged < 20 years were living with diabetes, and that each year approximately 15,000 youth aged < 20 years were diagnosed with type 1 diabetes and 3,700 with type 2 diabetes).11 The most recent update from the SEARCH researchers, released in 2012, shows data that type 2 diabetes in 10-to-19 year-olds had increased 21 percent between 2001 and 2009.8,12
Gestational diabetes’ cause is not known, but the American Diabetes Association (ADA) speculates that hormones secreted by the placenta block the action of the mother’s insulin in the body, resulting in insulin resistance and subsequent buildup of glucose levels. A 2014 analysis by the CDC indicates that the prevalence of gestational diabetes is as high as 9.2 percent.12
Rare types of diabetes include latent autoimmune diabetes in adults (LADA), maturity onset diabetes in the young (MODY), cystic fibrosis–related diabetes (CFRD), Cushing’s syndrome, and antiretroviral-associated diabetes. These diabetes types account for one percent to five percent of all diagnosed cases.13
Diabetes and chronic health conditions
Diabetes is illustrative of the chronic health conditions that are currently at the source of our healthcare challenges. This is primarily driven by the complexity and severity of the long-term complications of diabetes. In the undiagnosed or poorly managed patient, diabetes complications may be disabling and eventually life-threatening. Complications from diabetes include the following:14
- Cardiovascular disease, including coronary artery disease with chest pain (angina), heart attack, stroke, and narrowing of arteries (atherosclerosis).
- Nerve damage (neuropathy) leading to tingling, numbness, burning or pain that usually begins at the tips of the toes or fingers and gradually spreads upward, ultimately resulting in loss of sensation. For men, it may lead to erectile dysfunction.
- Kidney damage (nephropathy) that can lead to kidney failure or irreversible end-stage kidney disease, which may require dialysis or a kidney transplant.
- Eye damage (retinopathy) resulting in damage to the blood vessels of the retina (diabetic retinopathy), potentially leading to blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
- Foot damage as a result of nerve damage leading to cuts and blisters which may become seriously infected and may ultimately lead to toe, foot, or leg amputation.
- Skin conditions as a result of heighted susceptibility to bacterial and fungal infections.
- Hearing impairment
- Alzheimer’s disease. (Type 2 diabetes may increase the risk.)
A study published in the Journal of Medical Economics estimated the 2012 U.S. patient costs per acute event for the following major complications:15
- Cardiovascular disease: myocardial infarction $56,445; ischemic stroke $42,119; congestive heart failure $23,758; ischemic heart disease $21,406; and transient ischemic attack $7,388
- Kidney disease: $71,714 for end stage renal disease
- Eye disease: $2,862 blindness
- Nerve/foot damage: $9,041 for lower extremity amputations and $2,147 for diabetic foot ulcers.
Consider that, since 2012, healthcare costs have continued to escalate along with the number of individuals who have developed or are at risk for developing diabetes and associated chronic disease conditions as listed above. Through population management efforts, patients with diabetes or predisposition for diabetes can be identified, monitored, and managed in order to control disease, minimize the risk of complications, and reduce healthcare costs. And, indeed, these efforts begin with the laboratory.
HbA1c in diagnosis and monitoring of diabetes
Hemoglobin A1c (HbA1c) is made by the non-enzymatic attachment of glucose to the N-terminal valine of the ß-chain of hemoglobin. During the normal process of red blood cells dying and breaking down, the HbA1c is released. Consequently, the level of HbA1c is reflective of the average glucose concentration to which red blood cells were exposed over their eight-to-twelve- week life span.16 HbA1c had been customarily employed in the monitoring of diabetic patients and in guiding therapy. But with the ADA’s 2010 endorsement to use HbA1c as the main criterion for the diagnosis of type 2 diabetes, HbA1c was propelled to the limelight for its utility in both the screening for pre-diabetes and the diagnosis of diabetes.9,19,20
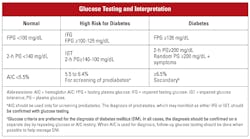
The endorsement by ADA was founded on data demonstrating that patients with HbA1c levels of 6.5 percent or greater had the same rate of retinopathy as those diagnosed using the standard criteria of fasting blood glucose and glucose tolerance testing9 (Table 1). HbA1c testing also provided key advantages over blood glucose testing including no requirement for fasting, sample draw convenience, and less susceptibility to variations in levels due to patient health, and analytical stability for laboratory testing.19 Some disadvantages of HbA1c were also considered, including increased cost and the potential to miss about 20 percent of patients with diabetes when compared to using fasting glucose and glucose tolerance testing. Additionally, HbA1c levels may vary due to patients’ race or ethnicity, and for conditions with abnormal red cell turnover, such as pregnancy, recent blood loss or transfusion, and some anemias, the diagnosis of diabetes must rely on blood glucose and not HbA1c.19
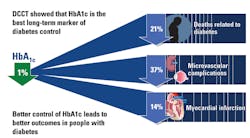
The International Experts Committee (IEC) had also recommended the use of HbA1c. However, the IEC recognized the lack of standardization that existed among the 100-plus methods available for HbA1c testing. The IEC recommended that the testing methodologies must be certified by the National Glycohemoglobin Standardization Program (NGSP) or traceable to the Diabetes Control and Complications Trial (DCCT) or UK Prospective Diabetes Study (UKPDS).16,17 The goal of the IEC was to ensure that the methods were able to generate highly similar results on a given blood sample. The NGSP was established by the American Association of Clinical Chemistry (AACC) to execute the protocol and establish the standardization process. The subsequent improvement in performance of HbA1c led to an increase in laboratories reporting HbA1c, from 50 percent in 1993 to approximately 99 percent by 2004, as well as simultaneous improvements in accuracy and reduced variability among laboratories.16,17
Laboratory-based HbA1c testing is well established, and numerous immunoassay, enzymatic, and ion exchange HPLC methods for HbA1c testing have been certified by NGSP. As of 2015, three POCT methods have also been certified.21 A primary advantage of HbA1c POCT, as well as glucose POCT, is expediting clinical decision by allowing providers to more quickly assess the efficacy of diabetes treatment and influence on health outcomes (Figure 4). This aids in the collective effort to lower a patient’s future HbA1c levels by enabling timely therapeutic modifications.21
The NGSP certification for POCT HbA1c tests does not mandate or account for end-user proficiency testing. However, proficiency testing materials are available from the College of American Pathologists (CAP). It is up to the specific healthcare setting to make the determination to participate in a proficiency program. Proficiency testing of POCT devices is recommended to ensure the integrity of test results and reduce testing errors.23
Alternate markers of glycemia
Fructosamine, glycated albumin, and 1,5-anhydroglucitol (1,5-AG) are three other available markers for glycemia.24
- Fructosamine reflects the average blood sugar concentration over the prior two to three weeks.
- Glycated albumin reflects mean glucose levels over the prior two to three weeks.
- 1,5-AG levels are associated with rapid glucose fluctuations and response within 24 hours.
For purposes of diagnosis and monitoring of diabetes, the alternate markers of glycemia are recommended to be used in conjunction with HbA1c. Presently, these markers may be best suited for testing in specific subsets of diabetic patients, such as those with variant hemoglobin, iron deficiency anemia, pregnancy, and chronic liver or kidney disease.24
Toward population management of diabetes
The burden of diagnosed and undiagnosed diabetes on the health of the U.S. population, coupled with the ever-escalating costs associated with disease management, treatment, and co-occurring conditions, can hardly be overstated. The CDC views the growing prevalence and incidence of diabetes as one of the most important public health issues of our time. Consequently, the CDC has published the “Compendium of Effective Public Health Strategies to Prevent and Control Diabetes” to educate the population on the consequences of diabetes and spearhead a call to action for screening and lifestyle improvements.25
Simultaneously, the Centers for Medicare and Medicaid Services (CMS) aims to address and curtail the burden of disease through population management initiatives, including pro-active screening, improved monitoring, and patient engagement in lifestyle changes. Risk factors such as obesity, high blood pressure, family history of diabetes, elevated lipid levels, and individuals over the age of 65 are eligible for screening. Medicare, Medicaid, and private payers advocate the pro-active screening of the general population for type 2 diabetes using such tests as HbA1c and blood glucose levels.
And so the laboratory and providers performing POCT play an integral part in facilitating the testing required to achieve the goals of the CDC, CMS, and private payers in reducing the burden of diabetes in the U.S. Screening for undiagnosed diabetes, management of diabetes, management of disease progression, and monitoring for co-occurring conditions and therapeutic efficacy are contingent on the availability and accessibility of standardized and accurate HbA1c and blood glucose testing.
REFERENCES
Clinical Chemistry. 2014;60(8):1062–1072.
Diabetes Spectrum. 2015;28(3):201-208.
Liana F. Romero PhD, MBA, MT(ASCP), serves as Senior Director, US Strategic Marketing and Clinical Affairs, within Siemens Healthcare US Laboratory Diagnostics. Dr. Romero is focused on connecting laboratory capabilities with hospital administration to navigate and thrive in the dynamic environment driven by healthcare reform, incentive programs, quality measurements, evolving reimbursement models, and hospital consolidation.