Diagnosing androgen deficiency in adult men
To earn CEUs, visit www.mlo-online.com under the CE Tests tab.
LEARNING OBJECTIVES
1. Identify the limitations that are currently problematic when diagnosing androgen deficiency.
2. Describe the signs and symptoms of androgen deficiency.
3. List ways in which the criteria for diagnosing androgen deficiency can be improved upon.
4. Identify the metabolites of testosterone and their possible use for future laboratory diagnostic value.
In recent years, there has been an explosive increase in prescriptions for testosterone replacement therapy (TRT) in adult men who are thought to have adult-onset hypogonadism (i.e., androgen deficiency [AD], also known as low testosterone or “low T”).1 This increase has been fueled by changing demographics and by increased public awareness of low T syndrome due to extensive advertising and numerous articles in the lay press. Despite recent controversies about risks for cardiovascular complications in men receiving TRT, the trend of increased testing and treatment for low T is likely to continue. Hence, it is imperative for clinical laboratory professionals to have a good understanding of this important topic.
The diagnosis and treatment of adult-onset hypogonadism in men older than 45 years of age remains controversial. For example, there is lack of consensus on the thresholds of testosterone that are needed to diagnose AD. Furthermore, evidence shows that testosterone levels in men decrease with age, at approximately one percent per year, beginning at about 40 years old. Because testosterone levels are known to decline as men grow older, there is debate about whether or not to interpret lower testosterone values in older men as being physiologic (i.e., a “normal” part of aging) or abnormal and worthy of treatment. For this reason, a standard approach in older men has been to interpret blood tests for testosterone in the context of the other clinical features of the patient in order to establish a diagnosis of androgen deficiency that should be treated.
Biology of testosterone
Testosterone is a steroid hormone that develops and maintains the primary and secondary sex characteristics in men (Figure 1). Its metabolites include estradiol (produced by aromatase enzyme found in fat and other tissues such as testes) and dihydrotestosterone (DHT)—an androgenic hormone that is approximately three to ten times more potent than testosterone.2,3 DHT is produced from testosterone by 5-alpha reductase, an enzyme that is found primarily in hair follicles, prostate, testes, and adrenal glands, but not in skeletal muscle.4
Measuring total testosterone
Total testosterone can be accurately measured by immunoassay and by mass spectroscopy.5 Even in men with severe deficiency of testosterone, enzyme immunoassays will provide accurate and reliable results. There is no clinical advantage to using mass spectroscopy for measuring total testosterone, although the results may be more precise and accurate at very low levels that are not normally seen even in hypogonadal men.5
In younger men, there is marked diurnal variation in testosterone levels, with the highest levels occurring in early morning upon awakening.6 The diurnal variation in total testosterone becomes less pronounced in older men.7 Nevertheless, current recommendations are that blood samples for total testosterone levels should be drawn before 10 a.m. in all men. There is currently no consensus regarding whether or not fasting is required, and most laboratories do not require it.
Total testosterone levels can vary considerably from day to day in the same man.8 Factors that can affect total testosterone on a day-to-day basis include sleep, diet, stress, illness, and exercise. Consequently, it is not advisable to make a diagnosis of low T on the basis of a single blood test result. Instead, two or even three tests taken on different days are recommended in order to ensure an accurate diagnosis.9
Lack of consensus on diagnostic criteria
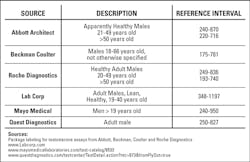
There are considerable variations in the reference intervals for total testosterone assays that are produced by various manufacturers of in vitro diagnostics and reference labs (Table 1). It is notable that the reference intervals are based on the range of values between the fifth and 95th percentiles of men of various ages. The populations of men that were used to derive these reference intervals are poorly defined with respect to age distribution and possible symptoms of low T, and it is unclear if these reference intervals provide a reliable basis for interpreting test results from men being tested for low T. Of particular concern are the lower limits of the reference intervals, which may be too low to identify the significant proportion of men who are truly hypogonadal but whose total testosterone levels still fall above the fifth percentile of the reference range.
Reference intervals for total testosterone levels reported by various reference laboratories also have considerable variation (Table 1). Once again, the variation is of particular concern at the low end of the reference interval, because many clinicians use this value to determine whether or not a man should be diagnosed as having low T.
An emerging approach to interpreting total testosterone levels in men is to use a clinical threshold cutoff value for the level. Based on recommendations from various sources,10-12 it appears that the clinical threshold for diagnosing low T probably lies somewhere between 300-500 ng/dL. Notably, this broad range lies considerably above the fifth percentiles for the testosterone values in Table 1. It should also be noted that all sources of the clinical thresholds recommend the primacy of clinical signs and symptoms when interpreting total testosterone values. For example, the Endocrine Society recommends “making a diagnosis of androgen deficiency only in men with consistent symptoms and signs and unequivocally low serum testosterone levels.”10 The American Urological Association goes even further and states that “there is no universally accepted threshold of T concentration that distinguishes eugonadal from hypogonadal men.”13
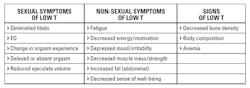
To resolve this conundrum, many experts now recommend that numerical values for total testosterone should be interpreted only in the context of the other clinical features of the patient. For this purpose, various clinical criteria for diagnosing or suspecting low T in men have been proposed (Table 2). Although all of these signs and symptoms are somewhat nonspecific, the sexual symptoms appear to be the most useful indicators of potential low-T. Consequently, in men older than 45 years of age who present with complaints of erectile dysfunction or other sexual problems, there should be a high index of suspicion for low T.
Testosterone binding and circulation
Testosterone circulates in the blood in a free (unbound) form and a bound form.14 Sex hormone-binding globulin (SHBG) and albumin are the primary sources of binding of testosterone. Approximately two percent of total testosterone circulates in the free form. Current thinking is that free testosterone is mostly responsible for the biological activity of the hormone, and the bound form is thought to be mostly inactive.
The free and bound forms can be directly measured by a variety of methods, or a mathematical formula can be used to calculate the percentage of free testosterone, based on the values for total testosterone, SHBG, and albumin.v15,16 Regardless of the method used to determine free testosterone, there is still substantial confusion and uncertainty regarding how to interpret the results. Some experts use both total testosterone and free testosterone to evaluate men presenting with symptoms of low T.
Effects of age and other factors
The levels of total testosterone in men decline gradually with age.17 By contrast, there is a much more pronounced decrease in free testosterone levels with age, which is probably due to a corresponding, age-related increase in SHBG levels. The reduced levels of free testosterone then stimulate secretion of higher levels of luteinizing hormone, which is the primary driver of testosterone synthesis in testes.
Other conditions besides aging also contribute to significant declines in testosterone in men older than 45 years of age. Chronic opioid use and obesity are two of the most significant drivers of reduced total testosterone.18,19 AIDS, hypertension, overtraining, certain medications, and diabetes are also associated with low T.20 Finally, there is emerging evidence that poor sleep quality and insufficient sleep are also associated with low T.21 Interestingly, poor sleep seems to be both a cause and an effect of low T.
Testing for dihydrotestosterone and estradiol
Testing for DHT levels is not a routine part of the workup for men being evaluated or treated for hypogonadism. At this time, it is not clear how to interpret the test results. It is likely that as our understanding of testosterone replacement therapy improves, there will be an increased interest in clinical testing for this metabolite of testosterone.
There is now considerable evidence that estradiol levels in men play an important role in modulating the effects of testosterone on sexual function, body fat, lean muscle mass, and bone density.11 Nevertheless, estradiol levels are still not commonly measured in men who are being evaluated or treated for low T. This is because the interpretive criteria for such testing are still not well understood. In some men, estradiol levels are measured in order to determine if testosterone therapy is causing an increase in estradiol due to aromatization of the testosterone. This can lead to symptoms of high estradiol such as bloating, fluid retention, and breast tenderness or gynecomastia.22 Some experts now recommend calculating a ratio of testosterone to estradiol, but this approach is not yet widely accepted. Nevertheless, it is likely that clinical laboratories will experience an increased demand for estradiol testing in men as our understanding and the prevalence of testosterone therapy increases.
Conclusion
From the preceding discussion, it should be apparent that our understanding of laboratory testing for low-T in men lags considerably behind the growing demand for testing and treatment of low T. Clinical laboratories, manufacturers of in vitro diagnostic tests, and clinicians should be aware of the many unanswered questions in this field. They should also begin to educate themselves about the important changes in this field that are likely to occur in the next few years.
REFERENCES
- Annual testosterone drug revenue in the U.S. in 2013 and 2018 (in billion U.S. dollars). http://www.statista.com/statistics/320301/predicted-annual-testosterone-drug-revenues-in-the-us/.
- Yeap BB, Alfonso H, Chubb SA, et al. In older men an optimal plasma testosterone is associated with reduced all-cause mortality and higher dihydrotestosterone with reduced ischemic heart disease mortality, while estradiol levels do not predict mortality. J Clin Endocrinol Metab. 2014;99:E9-18.
- Dias JP, Melvin D, Simonsick EM, et al. Effects of aromatase inhibition vs. testosterone in older men with low testosterone: randomized-controlled trial. Andrology. 2016;4: 33-40.
- Sato K, Iemitsu M. Exercise and sex steroid hormones in skeletal muscle. J Steroid Biochem Mol Biol. 2015;145 :200-205.
- Wang C, Catlin DH, Demers LM, Starcevic B, Swerdloff RS. Measurement of total serum testosterone in adult men: comparison of current laboratory methods versus liquid chromatography-tandem mass spectrometry. J Clin Endocrinol Metab. 2004;89:534-543.
- Crawford ED, Poage W, Nyhuis A, et al. Measurement of testosterone: how important is a morning blood draw? Curr Med Res Opin. 2015;31:1911-1914.
- González-Sales M, Barrière O, Tremblay PO, Nekka F, Desrochers J, Tanguay M. Modeling testosterone circadian rhythm in hypogonadal males: effect of age and circannual variations. AAPS J. 2016;18:217-227.
- Brambilla DJ, Matsumoto AM, Araujo AB, McKinlay JB. The effect of diurnal variation on clinical measurement of serum testosterone and other sex hormone levels in men. J Clin Endocrinol Metab. 2009;94:907-913.
- Bebb RA. Testosterone deficiency: practical guidelines for diagnosis and treatment. BCMJ. 2011;53:474-479.
- Bhasin S, Cunningham GR, Hayes FJ, et al. Task Force, Endocrine Society. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:2536-2559.
- Finkelstein JS, Yu EW, Burnett-Bowie SA. Gonadal steroids and body composition, strength, and sexual function in men. N Engl J Med. 2013;369:1011-1022.
- Morgentaler A, Khera M, Maggi M, Zitzmann M. Commentary: who is a candidate for testosterone therapy? A synthesis of international expert opinions. J Sex Med. 2014;11:2636-2645.
- Paduch DA, Brannigan RE, Fuchs EF, Kim ED, Marmar JL, Sandlow JI. The laboratory diagnosis of testosterone deficiency. Urology. 2014;83:980-8.
- Bhasin S, Jameson J. Disorders of the Testes and Male Reproductive System. In: Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J. eds. Harrison’s Principles of Internal Medicine, 19e. New York, NY: McGraw-Hill; 2015. http://accessmedicine.mhmedical.com/content.aspx?bookid=1130&Sectionid=79752467.
- Woodworth A, Lakhani V, Aleryani SL, Laposata M. The Endocrine System. In: Laposata M. eds. Laboratory Medicine: The Diagnosis of Disease in the Clinical Laboratory. New York, NY: McGraw-Hill; 2014. http://accessmedicine.mhmedical.com/content.aspx?bookid=1069&Sectionid=60777928.
- Ho CK, Stoddart M, Walton M, Anderson RA, Beckett GJ. Calculated free testosterone in men: comparison of four equations and with free androgen index. Ann Clin Biochem. 2006;43:389-397.
- Wu FC, Tajar A, Pye SR, et al. European Male Aging Study Group. Hypothalamic-pituitary-testicular axis in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab. 2008;93:2737-2745.
- Smith HS, Elliott JA. Opioid-induced androgen deficiency (OPIAD). Pain Physician. 2012;15(3 Suppl):ES145-156.
- Camacho EM, Huhtaniemi IT, O’Neill TW, et al. Age-associated changes in hypothalamic-pituitary-testicular function in middle-aged and older men are modified by weight change and lifestyle factors: longitudinal results from the European Male Ageing Study. Eur J Endocrinol. 2013;168:445-455.
- Kaltenboeck A, Foster S, Ivanova J, et al. The direct and indirect costs among U.S. privately insured employees with hypogonadism. J Sex Med. 2012;9:2438-2447.
- Wittert G. The relationship between sleep disorders and testosterone. Curr Opin Endocrinol Diabetes Obes. 2014;21:239-243.
- Tan RS, Cook KR, Reilly WG. High estrogen in men after injectable testosterone therapy: the low T experience. Am J Mens Health. 2015;9:229-234.