To take the test online go HERE. For more information, visit the Continuing Education tab.
LEARNING OBJECTIVES
Upon completion of this article, the reader will be able to:
1. Describe the goal of the “Guidelines and Recommendations for Laboratory Analysis in the
Diagnosis and Management of Diabetes Mellitus.”
2. List parameters of glycemic control in different populations of patients.
3. Discuss biologic and nonbiologic interferences of testing methods of HbA1c.
4. Describe methods of QA and patient management of the disease through different result strategies.
The recent “Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus”1-2 has not been as disruptive to the hemoglobin A1c (HbA1c) testing space as expected. The 16 HbA1c-related recommendations ((a)-(p) in the executive summary3) reflect current understanding of the diabetes testing environment and reaffirm and update previously established standards, making explicit the details only suggested before and indicating the future direction of industry best practices. This article will summarize the recommendations and explain the reasoning behind select guidelines and their repercussions within the testing laboratory.
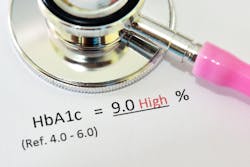
(a) Laboratory-based HbA1c testing can be used to diagnose (a) diabetes, with a value ≥6.5% (≥48 mmol/mol) diagnostic of diabetes, and (b) prediabetes (or high risk for diabetes) with an HbA1c level of 5.7% to 6.4% (39 to 46 mmol/mol). An NGSP-certified method should be performed in an accredited laboratory.
HbA1c is formed by slow, irreversible glycation of the N-terminal valine of hemoglobin’s beta globin chains. Accumulation in the blood reflects the patient’s average glycemic status over the previous 120 days. Normal glycemic control exhibits an HbA1c of <5.7%, while diabetics will have a value ≥6.5%. Values between these are pre-diabetic, with high risk for progression. HbA1c is not recommended for gestational diabetes screening, since faster recognition and treatment is required to avoid injury to mother or fetus.
(b) Recommendation: Point-of-care (POC) HbA1c testing for diabetes screening and diagnosis should be restricted to FDA-approved devices at CLIA-certified laboratories that perform testing of moderate complexity or higher.
This guideline highlights concerns about the accuracy of POC methods. Their exemption from proficiency testing (CLIA waived) prevents regular collection of HbA1c survey data by these methods. Evaluating them through publications, the guidelines quote several meta-analyses4-6 showing unacceptable bias and large coefficient of variation (CVs) in current POC devices. Stipulating FDA approval and use at CLIA-certified moderate-complexity labs overcomes this by requiring documentation of objective and ongoing acceptable performance.
(c) HbA1c should be measured routinely (usually every 3 months until acceptable, individualized targets are achieved and then no less than every 6 months) in most individuals with diabetes mellitus to document their degree of glycemic control.
(d) Treatment goals should be based on ADA recommendations which include maintaining HbA1c concentrations <7% (<53 mmol/mol) for many nonpregnant people with diabetes and more stringent goals in selected individuals if this can be achieved without significant hypoglycemia or other adverse effects of treatment. (Note that these values are applicable only if the assay method is certified by the NGSP as traceable to the DCCT reference.)
(e) Higher target ranges are recommended for children and adolescents, and are appropriate for individuals with limited life expectancy, extensive co-morbid illnesses, a history of severe hypoglycemia, and advanced complications.
The clinical use of HbA1c% is in diabetic monitoring regarding the long-term vascular damage of chronic complications: neuropathies, retinopathy, kidney failure, diabetic ulcers, heart damage, and increased incidence of stroke. The <7% target minimized progression of chronic diabetic complications in landmark studies7-8 balanced against the hazards of acute hypoglycemia. However, this update suggests promotion of “personalized” targets for some population subsets, accounting for differences in risk and clinical condition, allowing more stringent or relaxed targets, including:
(f) During pregnancy and in preparation for pregnancy, women with diabetes should try to achieve HbA1c goals that are more stringent than in the nonpregnant state, aiming ideally for <6.0% (<42 mmol/mol) during pregnancy to protect the fetus from congenital malformations and the baby and mother from perinatal trauma and morbidity owing to large-for-date babies.
Diabetics during pregnancy have a more stringent (<6.0%) target, due both to fetal risk and to increased erythropoietin levels accelerating RBC turnover,9 depleting HbA1c in the bloodstream. This accounts for pregnant patients’ HbA1c% reflecting glycemic status differently. A pregnant, diabetic patient might have an HbA1c of 6.5 %, which is below the standard <7.0%, but, for them, indicative of poorly controlled diabetes. Recognition that an analyte reflects conditions differently in some patients aligns with the current trends of personalized medicine.
(g) Laboratories should be aware of potential interferences, including hemoglobin variants that may affect HbA1c test results depending on the method used. In selecting assay methods, laboratories should consider the potential for interferences in their particular patient population.
This raises several questions: What is required of the lab? Can labs with a low diversity patient population ignore this guideline? What diversity threshold is low enough? Numerous studies document HbA1c testing of inappropriate patients, although rates differ widely.10-11 One pulled a random sampling of their lab’s HbA1c orders and found sufficient S/S, S/C, and S/Beta-thalassemia patients to project 2,000 to 3,000 improperly ordered samples per year.10 These guidelines suggest checking the National Glycohemoglobin Standardization Project (NGSP) interferences website and reading limitations in manufacturer product instructions. Labs may be surprised by the cautions they find: Some immunoassays warn about high Hb F (>10%) artificially lowering measured HbA1c, and state “care must be taken” with variants;12-15 other versions cautioning against diagnosis or monitoring in sickle trait patients .16 Other enzymatic methods warn against high HbF interference without defining “high” and caution against use in trait patients except where it’s been proven to have no influence on results.17
The NGSP website acknowledges inherent HbF interference by certain methodologies, stating “In the absence of specific method data, it can generally be assumed that immunoassay, boronate affinity and enzymatic methods show interference from elevated Hb F levels.”18 The irony of these cautions in non-separation methodologies (HbA1c% produced without an Hb profile) is that they cannot see interferences, raising the alarm only for results outside the physiologic range. Separation techniques (CE-HPLC or capillary electrophoresis) display the separated hemoglobin fractions with their result, enabling better detection and evaluation of interferences, some even flagging abnormalities for review. Hb F has less impact as a result in these methods,18 e.g., capillary electrophoresis finds no interference for HbF<23% due to the isolation of the HbF peak from HbA0 and HbA1c,19 and rare variants co-migrating and distorting the HbA0 or HbA1c peaks trigger safeguards blocking result calculation, preventing misreporting events. However, there are other reasons to recognize variants in diabetes testing:
(h) HbA1c measurements in individuals with disorders that affect red blood cell turnover may provide spurious (generally falsely low) results regardless of the method used and glucose testing will be necessary for screening, diagnosis, and management.
Shortening the average 120-day RBC lifespan lowers equilibrium HbA1c%, as hemoglobin will have less blood glucose exposure, counter-indicating its standard use in diabetic management. This is not a method-dependent analytical interference, but a biological one, suppressing HbA1c accumulation. All current methodologies warn against these misleading values, listing conditions like hemolytic anemia, blood loss, transfusion, iron deficiency, and spherocytosis.12-16,19 Hemoglobinopathies, typically evident by separation methods but invisible to non-separation methods, may also impact RBC lifespan or glycation rates. Although the NGSP website declares few interferences from common variants,18 this covers analytical interference, not biological. Hb S trait, typically clinically silent (and frequently undiagnosed), has historically been shown to significantly accelerate RBC turnover,20-21 likely linked to the reduced HbA1c% in this population,22 and leading the American Diabetes Association to note “…it seems prudent to establish A1C goals in these [sickle trait and other] populations with consideration of individualized CGM, BGM, and A1C results.”23 Thalassemias, mutations limiting hemoglobin production, similarly accelerate RBC turnover,24-25 and may be incidentally detected in some HbA1c methods — capillary electrophoresis visualizes a non-reportable but indicative HbA2, whose gross elevation could indicate beta thalassemia. These incidental discoveries alert clinicians to possible HbA1c discrepancies.
(i) Assays of other glycated proteins, such as fructosamine or glycated albumin, may be used in clinical settings where abnormalities in red blood cell turnover, hemoglobin variants, or other interfering factors compromise interpretation of HbA1c test results, although they reflect a shorter period of average glycemia than HbA1c.
(j) HbA1c cannot be measured and should not be reported in individuals who do not have Hb A, e.g., those with homozygous hemoglobin variants, such as Hb SS or Hb EE; glycated proteins, such as fructosamine or glycated albumin, may be used.
A patient without native HbA cannot produce HbA1c. Any HbA1c reporting in this patient is analytically and fundamentally incorrect. Non-separation methodologies are incapable of distinguishing between HbA1c and most glycated variants, reporting values even in homozygous or doubly heterozygous beta variant patients. Accelerated RBC turnover or glycated variant mismatch may drive test results non-physiologically low, but those with milder impact may go undetected, possibly causing misdiagnosis noted in case studies.26-31 Separation techniques uncovering non-A patients may flag the patient or be incapable of providing results, an in-test safety factor. When biological or analytical interferences impact an HbA1c result, other glycated proteins can be used as a second-best option.
(k) Laboratories should use only HbA1c assay methods that are certified by the NGSP as traceable to the DCCT reference. The manufacturers of HbA1c assays should also show traceability to the IFCC reference method.
Prescribed target values assume that all assays employ the same scale correlating HbA1c to diabetic complication risk. Manufacturers prove this by showing traceability to the IFCC HbA1c% reference method, but approaches vary widely. Immunoassay and enzymatic methods measure HbA1c by targeting glycation site epitopes, excluding glycated-HbF but including variants if mutations are located elsewhere. “Total HbA” is approximated based on spectroscopic analysis or optical methods (respectively) that pool all hemoglobins, skewing the formula in the presence of abnormal production. Boronate Affinity sorts hemoglobins into “glycated” and “non glycated’ fractions, deriving HbA1c% from a curve fit not accounting for any abnormal Hbs. HPLC is more discriminating, as variant structures anywhere within a hemoglobin may shift elution time. However, incidental separation of a myriad of “HbA total” subspecies (labile, acetylated, etc.) requires careful re-collection, occasionally complicated by co-eluting rare variants.32-34 Capillary electrophoresis minimizes these complications, simplifying the pattern through migration fine tuning, gathering extraneous fractions together while separating variants, and allowing HbA1c and total HbA quantification by the same detection method.
(l) Laboratories that measure HbA1c should participate in an accuracy-based proficiency-testing program that uses fresh whole blood samples with targets set by the NGSP Laboratory Network.
Proficiency testing provides essential method quality checks for certified laboratories. In providing samples with established HbA1c IFCC reference method results (methods impractical in clinical labs), the pooled participant results evaluate method variance and bias, although Hb variants are typically neglected.
(m) The goals for imprecision for HbA1c measurement are intra-laboratory CV <1.5% and inter-laboratory CV <2.5% (using at least 2 control samples with different HbA1c levels), and ideally no measurable bias.
These guideline CVs, a significantly tightening from prior guidelines (2% and 3.5%, respectively),35 mean that two successive patient samples differing by 0.5% have a 95% chance of reflecting a real change in glycemic status, rather than random instrument scatter. Comparison with current CAP (a popular proficiency testing resource) data36 where ±6% is the acceptable limit, highlights the new guideline’s stringency. Comparison with the EuroA1c project (a European-centered program involving 22 nations) shows that CV<2.5% lands within the “silver medal” range, a triumph consistently achieved by only few methodologies.37
(n) HbA1c should be reported as a percentage of total hemoglobin or as mmol/mol of total hemoglobin.
(o) HbA1c may also be reported as estimated average glucose (eAG) to facilitate comparison with the home glucose monitoring results and make the interpretation of the HbA1c more accessible to people with diabetes.
HbA1c% values are used in the United States; mmol/mol is used throughout Europe and much of the rest of the world. However, patients require connection between the infrequently measured HbA1c and their daily glycometer reading to better manage dietary choices, insulin regiment, and alleviate anxiety about their disease progression. Offering an eAG value in parallel with their A1c result can provide this connection.
(p) Laboratories should verify by repeat testing specimens with HbA1c results below the lower limit of the reference interval or greater than 15% (140 mmol/mol) HbA1c.
Regulating responses to non-physiologic results serves two purposes: troubleshooting instrument malfunction, and as a fail-safe against misreporting samples with interferences. Upon retesting, a changed result indicates instrument malfunction, and an identically repeated result indicates a hemoglobinopathy or other interference should be suspected. While important for all HbA1c methods, this is essential for the non-separation methodologies as the sole interference failsafe, while separation methods’ visualizing of unusual hemoglobin profiles can detect many interferences even without the numerical result review.
These guidelines, while reaffirming the prior version,35 expand upon advice to watch for “marked discordance between measured A1c and plasma glucose levels,”35 indicating either analytical interferences or conditions that “alter the relationship between A1c and glycemia.” The new guidelines set tighter standards, make explicit the potential for misleading results, and define patients for whom the test is absolutely inappropriate. Previously cautioning against diagnosis by HbA1c in certain patients, now any HbA1c reporting at all is strongly discouraged in the presence of analytical interference, biological interference, or conditions of altered RBC turnover. These recommendations are in alignment with HbA1c assay package inserts stating they are not appropriate for use in patients without hemoglobin A or even in the diagnosis of patients with trait hemoglobinopathies. In conclusion, the arc of the regulatory environment defined by these updated guidelines is leaning heavily toward personalized goals for specific diabetic patients and issues that are clearly addressable only by separation methods.
References
1 Sacks DB, Arnold M, Bakris GL, et al. Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus. Clin Chem. 2023;2;69(8):808-868. doi:10.1093/clinchem/hvad080.
2 Sacks DB, Arnold M, Bakris GL, et al. Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus. Diabetes Care. 2023;1;46(10):e151-e199. doi:10.2337/dci23-0036.
3 Sacks DB, Arnold M, Bakris GL, et al. Executive Summary: Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus. Diabetes Care. 2023;1;46(10):1740-1746. doi:10.2337/dci23-0048.
4 Lenters-Westra E, Slingerland RJ. Six of eight hemoglobin A1c point-of-care instruments do not meet the general accepted analytical performance criteria. Clin Chem. 2010;56(1):44-52. doi:10.1373/clinchem.2009.130641.
5 Hirst JA, McLellan JH, Price CP, et al. Performance of point-of-care HbA1c test devices: implications for use in clinical practice - a systematic review and meta-analysis. Clin Chem Lab Med. 2017;1;55(2):167-180. doi:10.1515/cclm-2016-0303.
6 Nathan DM, Griffin A, Perez FM, et al. Accuracy of a Point-of-Care Hemoglobin A1c Assay. J Diabetes Sci Technol. 201913(6):1149-1153. doi:10.1177/1932296819836101.
7 Diabetes Control and Complications Trial Research Group; Nathan DM, Genuth S, Lachin J, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;30;329(14):977-86. doi:10.1056/NEJM199309303291401.
8 Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;12;352(9131):837-53.
9 Lurie S, Mamet Y. Red blood cell survival and kinetics during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2000;93(2):185-92. doi:10.1016/s0301-2115(00)00290-6.
10 Rhea JM, Koch D, Ritchie J, et al. Unintended reporting of misleading Hb A(1c) values when using assays incapable of detecting hemoglobin variants. Arch Pathol Lab Med. 2013;137(12):1788-91. doi:10.5858/arpa.2012-0714-OA.
11 Latzig DL, Baynes SC, Feuerhake T, Gunsolus IL. Evaluation of local hemoglobinopathy prevalence and promotion of accurate hemoglobin A1c testing using historical data retrieval. Clin Biochem. 2023;114:59-62. doi:10.1016/j.clinbiochem.2023.02.001.
12 Roche Diagnostics, GmbH. Tina-quant Hemoglobin A1c Gen.3-Whole Blood and Hemolysate Application Order Information (cobas c 111) 2022-02, V3.0 English 1-6.
13 Roche Diagnostics, GmbH. Tina-quant Hemoglobin A1c Gen.3-Whole Blood Application – Standardized according to IFCC transferable to DCCT/NGSP Order Information (COBAS INTEGRA 400 plus) 2022-02, V3.0 English 1-6.
14 Roche Diagnostics, GmbH. Tina-quant Hemoglobin A1c Gen.3-Whole Blood Application Order Information (cobas c 311, cobas c 501/502) 2022-02, V3.0 English 1-6.
15 Beckman Coulter, Inc. USA. AU US Instructions For Use (AU400/AU480, AU640e/680, AU2700/AU5400/AU5800 and DxC 700 AU Beckman Coulter Analyzers) 2020 1-19.
16 Roche Diagnostics, GmbH. Tina-quant Hemoglobin A1cDx Gen.3 2021-02, V1.0 English.
17 Siemens Healthcare Diagnostics Inc. USA. Enzymatic Hemoglobin A1c (A1c_E) High-Volume Assay (Atellica CH Analyzer) 2021; Revy.03:1-20.
18 HbA1c Assay Interferences. Ngsp.org. Accessed March 25, 2024. https://ngsp.org/interf.asp.
19 Sebia France. Capi 3 Hb A1c Using the Capillarys 3 Tera Instrument Family. (US English release) 2019 1-23.
20 McCurdy PR. 32-DFP and 51-Cr for measurement of red cell life span in abnormal hemoglobin syndromes. Blood. 1969;33(2):214-24.
21 SUAREZ RM, BUSO R, MEYER LM, OLAVARRIETA ST. Distribution of abnormal hemoglobins in Puerto Rico and survival studies of red blood cells using Cr51. Blood. 1959;14(3):255-61.
22 Lacy ME, Wellenius GA, Sumner AE, et al. Association of Sickle Cell Trait With Hemoglobin A1c in African Americans. JAMA. 2017;7;317(5):507-515. doi:10.1001/jama.2016.21035.
23 ElSayed NA, Aleppo G, Aroda VR, et al. 6. Glycemic Targets: Standards of Care in Diabetes-2023. Diabetes Care. 2023;1;46(Suppl 1):S97-S110. doi:10.2337/dc23-S006.
24 Guimarães JS, Cominal JG, Silva-Pinto AC, et al. Altered erythropoiesis and iron metabolism in carriers of thalassemia. Eur J Haematol. 2015;94(6):511-8. doi:10.1111/ejh.12464.
25 Fucharoen S, Viprakasit V. Hb H disease: clinical course and disease modifiers. Hematology Am Soc Hematol Educ Program. 2009:26-34. doi:10.1182/asheducation-2009.1.26.
26 Karimi SS, Jin M, Murga-Zamalloa C. Analytical and Clinical Significance of Rare Hemoglobin Variants during HbA1c Monitoring in Patients with Diabetes Mellitus: Two Cases of Hemoglobin G-Ferrara and Hemoglobin G-Copenhagen in Diabetic Patients with Sickle Cell Trait. J Appl Lab Med. 2023;6;8(2):407-412. doi:10.1093/jalm/jfac135.
27 Higgins T, Stewart D, Boehr E. Challenges in HbA1c analysis and reporting: an interesting case illustrating the many pitfalls. Clin Biochem. 2008;41(13):1104-6. doi:10.1016/j.clinbiochem.2008.06.005.
28 Adekanmbi J, Higgins T, Rodriguez-Capote K, et al. Erroneous HbA1c results in a patient with elevated HbC and HbF. Clin Chim Acta. 2016;1;462:153-157. doi:10.1016/j.cca.2016.09.017.
29 Kangastupa P, Åkerman K, Risku S, et al. The prevalence of hemoglobin Tacoma in Finland detected by HbA1c capillary electrophoresis. Scand J Clin Lab Invest. 2023;83(1):51-57. doi:10.1080/00365513.2022.2164739.
30 Rhea JM, Molinaro R. Pathology consultation on HbA(1c) methods and interferences. Am J Clin Pathol. 2014;141(1):5-16. doi:10.1309/AJCPQ23GTTMLAEVL.
31 Shimizu S, Taira A. Two Non-diabetic Cases of Variant Hemoglobin Treated with Oral Hypoglycemic Agents Due to Spurious HbA1c Elevation. J Jpn Diabetes Soc. 2015;58(2):121-127.
32 Van Den Ouweland J, Van Daal H. The silent hemoglobin alpha chain variant Hb Riccarton [alpha51(CE9)Gly-->Ser] may affect HbA1c determination on the HLC-725 G7 analyzer. Clin Chem Lab Med. 2008;46(6):827-830.
33 Yang X, Zeng X, Zhang Y, Kuang W, He D. Evaluation of interference from 16 hemoglobin variants on hemoglobin A1c measurement by five methods. Scand J Clin Lab Invest. 2023;83(1):18-22. doi: 10.1080/00365513.2022.2155990.
34 Rodríguez-Capote K, Estey MP, Barakauskas VE, et al. Identification of Hb Wayne and its effects on HbA1c measurement by 5 methods. Clin Biochem. 2015;48(16-17):1144-50. doi:10.1016/j.clinbiochem.2015.07.100.
35 Sacks DB, Arnold M, Bakris GL, et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabetes Care. 2011;34(6):e61-99. doi:10.2337/dc11-9998.
36 NGSP CAP Survey Data. Ngsp.org. Accessed March 25, 2024. https://ngsp.org/CAPdata.asp.
37 EurA1c trial. Ifcchba1c.org. Accessed March 25, 2024. https://www.ifcchba1c.org/GeneralInformation.aspx?I=17.
To take the test online go HERE. For more information, visit the Continuing Education tab.